
During 2020, depressive disorders are anticipated to become the second leading contributor to the global burden of disease, a startling milestone that holds the number #1 spot of global disabilities and affects more than 340 million people each year (Greden, 2001).
Depressive disorders have high rates of crossover with other mental health difficulties, including psychosis and anxiety; 25% of those with schizophrenia and 81% of patients with generalised anxiety disorder also have depression (Brinsley et al., 2020). This alarming association extends into physical disorders as well, with 65% of people suffering from depression also having a physical condition, such as cardiovascular disease or diabetes type II (Vancampfort et al., 2015).
In recent years, physical activity has been highlighted by researchers for its beneficial uses in both mental and physical health (Brinsley et al., 2020). Despite the discovery, there still is little evidence of the usage of exercise as an intervention in standard care (Schuch et al., 2017).
Yoga has become increasingly popular in Western culture for its benefits in reducing anxiety and stress, while consistent sessions have shown to produce positive physical effects, including slowing the progression of heart disease (Link, 2017). Could yoga reduce depressive symptoms as well?
In a recent study published in the British Journal of Sports Medicine, Brinsley and colleagues (2020) sought to uncover this mystery for a multitude of mental disorders. In addition, they investigated the physical health outcomes that yoga can produce for patients with mental disorders.

Can yoga reduce depressive symptoms in mental disorders?
Methods
Researchers conducted a systematic review and a meta-analysis of previous studies that have used yoga intervention as a treatment for patients with mental disorders. They searched various databases with the keywords “mental disorders” “mental disease” and “yoga” for adult patients 18 and older with a diagnosed mental disorder under the conditions of Diagnostic and Statistical Manual of Mental Disorders (DSM) 3, 4, 5 guidelines. Mental disorders included in the search were depressive disorders, anxiety disorders, affective disorders, trauma disorders, psychotic disorders, panic disorders, and alcohol and substance use disorders.
In each intervention, yoga had to encompass more than 50% of the total intervention and only Randomised Controlled Trials (RCTs) were eligible for inclusion. The study quality was analysed using the PEDro checklist and 35% of the studies used were checked for quality assurance.
Results
Based on the search criteria, 19 studies were included in the final analysis, comprising of 1,080 participants in total. The patient profiles for the trials were quite diverse:
- 9 trials included patients with a depressive disorder
- 5 trials were included with patients who had a diagnosis of schizophrenia
- 1 trial had patients with alcohol dependency
- 1 trial included a range of psychiatric disorders all in one intervention
- 69% of all study participants were women
Primary results
- There was a moderate reduction in depressive symptoms in 9 different mental disorders when a yoga intervention was used in comparison to control groups
- No reduction in depressive symptoms was found in PTSD trials, but 1 study found that 52% of participants no longer had clinically significant PTSD in comparison to controls (van der Kolk et al., 2014)
- There was a small reduction in alcohol dependency disorders, but it was not statistically significant (p=.69)
- There was a large effect observed in all 5 trials of participants with schizophrenia
- The frequency of sessions attended weekly was associated with a greater reduction in depressive symptoms.
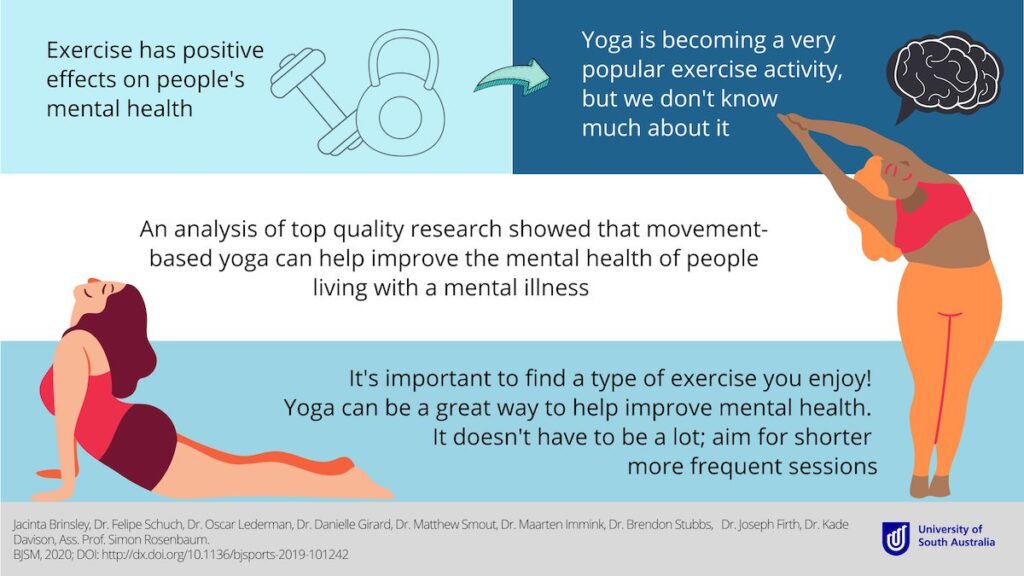
Researchers indicated a moderate reduction in depressive symptoms in a range of mental disorders when physically active yoga sessions were used.
Conclusions
Two main findings were highlighted as most notable by the researchers:
- A moderate reduction in depressive symptoms in a range of mental disorders was suggested when physically active yoga intervention was utilised
- There was a “dose-response relationship” between the frequency of yoga sessions and the reduction of depressive symptoms.
Based on the results of the review, the authors of the study indicated that health care providers and clinicians should consider the beneficial use of yoga as a treatment for mental health disorders. They also highlighted the necessity to conduct further research to evaluate yoga compared to other conventional forms of exercise.
Researchers found a dose-response relationship between yoga sessions and reduction of depressive symptoms: the higher the frequency of sessions attended, the greater reduction in symptoms.
However, as we have said in previous elf blogs about yoga, the quality of the trials in this field is quite poor. This review once again confirms this, with the reviewers finding that most of the studies included in their review having poor methodological quality, with inadequate blindness of assessors, inadequate follow-up, and a mixture of interviewer rated and self-reported outcomes (Brinsley et al., 2020).

The frequency of sessions attended weekly was associated with a greater reduction in depressive symptoms.
Strengths and limitations
In the past, several systematic reviews and meta-analysis have assessed yoga interventions for their therapeutic effects in mental disorders (Cramer et al., 2013; Pilkington et al., 2005). However, to the authors’ knowledge, no study has ever analysed the transdiagnostic benefits of yoga until the current review (2020). Researchers did not focus solely on one mental health disorder but a variety of psychiatric conditions, to truly assess how beneficial yoga interventions can be for specific clinical populations.
Despite the review’s strengths, there are still significant limitations. A range of yoga interventions were used in the trial, however, only 19 studies were included out of 80 that were originally found in the search based on the author’s removal of duplicate articles and predetermined eligibility criteria, which hugely limited the total number of participants. Also, researchers chose trials with poorly defined yoga interventions and did not always know the composition of each yoga session. For example, there seemed to be uncertainty about whether the trial included mindfulness, meditation, or physical activity-based yoga sessions. Furthermore, only 35% of the studies used were checked for quality assurance using the PEDro checklist, a significantly low number in terms of assessing methodological soundness. Because of this, researchers found that most of the studies chosen had poor methodological quality, with inadequate blindness of assessors, inadequate follow-up, and a mixture of interviewer rated and self-reported outcomes (Brinsley et al., 2020).
Higher-quality studies with a large and adequate sample size should be conducted with well-defined yoga interventions within each chosen trial. If these key changes are made, an updated systematic review has the potential to influence how psychiatrists and clinicians view the uses of yoga for people with depression that is comorbid with other mental illnesses.

The quality of the research about yoga and mental illness still leaves something to be desired. More high quality trials are needed.
Implications for practice
One in four people worldwide will experience a mental disorder at some point in their lifetime, and with such a high global burden of disease, there is a clear need for an effective intervention that is accessible to everyone (WHO, 2019).
This review provides promising evidence for the usability of physical activity, specifically yoga, as a treatment for mental disorders in clinical practice, but the quality of the research is not currently sufficient for this to become mainstream practice. One of the great things about yoga as an intervention is that it is accessible everywhere and to everyone. One can find a multitude of sessions at their local gym, specialised yoga studios, or even from the comfort of their own home with over 1 million YouTube videos devoted to yoga and its practices. All you need is some floor space.
The accessibility of yoga has the potential to enable clinicians to suggest physical yoga sessions for their patients, especially short and daily sessions, since results show higher frequency greatly reduces depressive symptoms. However, in clinical practice, extrapolating a specific yoga “dosage” that produces the most optimal benefits for patients would inform clinicians even further, and provide a starting point on how treatment with yoga could be “prescribed.”
Given the current state of the world, from being isolated at home during a global pandemic, to witnessing the atrocities being committed against black people worldwide, mental health disorders are being exacerbated in many people, and understandably so. Researchers admit that yoga is not a solve-all method of treatment, however it can provide a source of peace from the daily struggles that we are all experiencing. I’ve personally started 20-minute sessions of physically active yoga in the hope that I can find some Zen through these uncertain times.
Namaste!
There’s a clear need for an easily accessible, effective intervention for depressive disorders. Could yoga be the answer for some people?
Statement of interests
None.
Links
Primary paper
Brinsley, J., Schuch, F., Lederman, O., Girard, D., Smout, M., Immink, M. A., … Rosenbaum, S. (2020). Effects of yoga on depressive symptoms in people with mental disorders: a systematic review and meta-analysis. British Journal of Sports Medicine.
Other references
Cramer, H., Lauche, R., Langhorst, J., & Dobos, G. (2013). Yoga For Depression: A Systematic Review And Meta-Analysis. Depression and Anxiety, 30(11), 1068–1083.
Greden, J. F. (2001). The Burden of Recurrent Depression: Causes, Consequences, and Future Prospects. Retrieved from https://www.researchgate.net/publication/11750034_The_Burden_of_Recurrent_Depression_Causes_Consequences_and_Future_Prospects
Link, R. (2017, August 30). 13 Benefits of Yoga That Are Supported by Science. Retrieved from https://www.healthline.com/nutrition/13-benefits-of-yoga
NHS. (2020). Mental Health. Retrieved from https://www.england.nhs.uk/mental-health/
Pilkington, K., Kirkwood, G., Rampes, H., & Richardson, J. (2005). Yoga for depression: The research evidence. Journal of Affective Disorders, 89(1-3), 13–24.
Prathikanti, S., Rivera, R., Cochran, A., Tungol, J. G., Fayazmanesh, N., & Weinmann, E. (2017). Treating major depression with yoga: A prospective, randomized, controlled pilot trial. Plos One, 12(3).
Schuch, F., Vancampfort, D., Firth, J., Rosenbaum, S., Ward, P., Reichert, T., … Stubbs, B. (2017). Physical activity and sedentary behavior in people with major depressive disorder: A systematic review and meta-analysis. Journal of Affective Disorders, 210, 139–150.
Uebelacker, L. A., Bailey, G., Herman, D., Anderson, B., & Stein, M. (2016). Patients Beliefs About Medications are Associated with Stated Preference for Methadone, Buprenorphine, Naltrexone, or no Medication-Assisted Therapy Following Inpatient Opioid Detoxification. Journal of Substance Abuse Treatment, 66, 48–53.
Vancampfort, D., Stubbs, B., Mitchell, A. J., Hert, M. D., Wampers, M., Ward, P. B., … Correll, C. U. (2015). Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: a systematic review and meta-analysis. World Psychiatry, 14(3), 339–347.
Van der Kolk, B. A. V. D., Stone, L., West, J., Rhodes, A., Emerson, D., Suvak, M., & Spinazzola, J. (2014). Yoga as an Adjunctive Treatment for Posttraumatic Stress Disorder. The Journal of Clinical Psychiatry, 75(06).
WHO. (2013, July 29). Mental disorders affect one in four people. Retrieved from https://www.who.int/whr/2001/media_centre/press_release/en/
Photos
- Photo by kike vega on Unsplash
- Photo by Simon Rae on Unsplash
- Photo by Anupam Mahapatra on Unsplash
- Photo by Amanda Jones on Unsplash
