
cWe all know that depression is common, affecting about one in 20 adults worldwide (Institute of Health Metrics and Evaluation, 2019), meaning that around 280 million people have a diagnosis of depression. Even more common are those experiencing depression symptoms affecting more than one in 10 people (Zhang et al., 2022). This is worrying, given that symptoms such as low mood, lack of enjoyment, motivation, and achievement, impact significantly on functioning and healthcare utilisation (Lee et al., 2019) and increase the risk of subsequently developing major depression (Zhang et al., 2022).
Treating depression effectively is a global priority. Various treatments can be used, including psychological treatments like Cognitive Behaviour Therapy (CBT) and antidepressant medication (sometimes referred to as a pharmacological treatment). Addressing the global burden of depression is a priority covered by the World Health Organisation’s Mental Health Gap Action Programme and investing in scaling-up treatments for depression has been shown to lead to a four-fold return in improved health and ability to work (Chisholm et al., 2016) meaning there is a strong economic argument for investing in effective treatments for depression. Knowing which treatments work best (i.e., are most effective) and in what forms, is of great interest to people experiencing depression, therapists offering treatment, and those planning service delivery.
There are many original studies reporting on comparisons of one treatment to another (or to a waiting list), and meta-analyses systematically and statistically comparing findings from similar trials. Arguably, Cuijpers et al. (2023) analysis is the most useful summary yet of all the available information aiming to answer the question of how Cognitive Behavioural Therapy (CBT) compares to all the other treatment options and in what formats for whom. One paper to answer multiple questions!

Is CBT more effective than other pharmacological and psychological treatments for depression across the lifespan?
Methods
The authors conducted a meta-analysis, a highly regarded method to synthesise research findings across multiple trials. Four large databases and references of previous reviews were searched for randomised controlled trials which included terms related to ‘depression’ or ‘psychotherapy’. The resulting studies were screened so only those which compared CBT to other psychotherapies, pharmacological treatments, a combination of the two, or a control condition (e.g., waitlist, care as usual) were included.
Each of the studies was further separated into groups, including the type of control group used, the method used to deliver CBT (e.g. individual, group, telephone, guided self-help, and unguided self-help), the comparison group (e.g., psychotherapies, pharmacological, combined), for participants that were inpatients, and for participants who were children and adolescents. Multiple analyses were then run on these groups to help understand how effective the different formats were, with each comparison reporting the number needed to treat (NNT) to give an impact measure. Further sensitivity analysis such as only including low risk of bias and publication bias corrections were carried out.
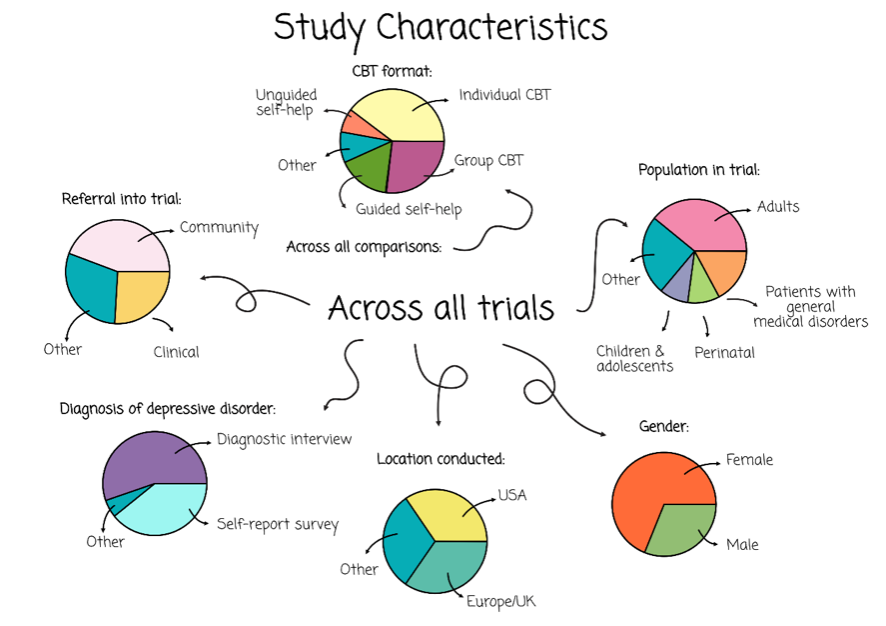
Additionally, a quality assessment was completed for each of the studies to consider the quality of the included studies and a score out of 4 (with 4 being the highest) was given. Recorded characteristics included the participants in the studies (e.g., age, method to diagnose, males vs females), the CBT (e.g., number of sessions) and study format (e.g., date of publication, country it was conducted in).
Results
From the search, 30,889 trials were identified, and of them, 409 trials met the criteria to be included. The sum of the participants from these trials amounted to 52,702 people, 27,000 of whom received CBT. An overview of the population included across the studies includes a 69% female to male divide and a mean age of 40.1 years with only 9% of trials including children. Most trials were carried out in the USA, UK, or Europe.
All 409 trials were scored for quality assessment, with scores ranging from four to zero. 32% of the studies achieved 4 and 26% achieved 0 or 1. This means we need to be cautious about the conclusions we draw, especially from studies with a higher risk of bias (scoring 0 or 1). Therefore, we reported the results when the analysis was run with all trials included (where appropriate) and when only the highest scoring trials for low risk of bias were included (i.e., scoring 4).
30,889 trials were identified, and of them, 409 trials met the criteria to be included in the study. View full size image.
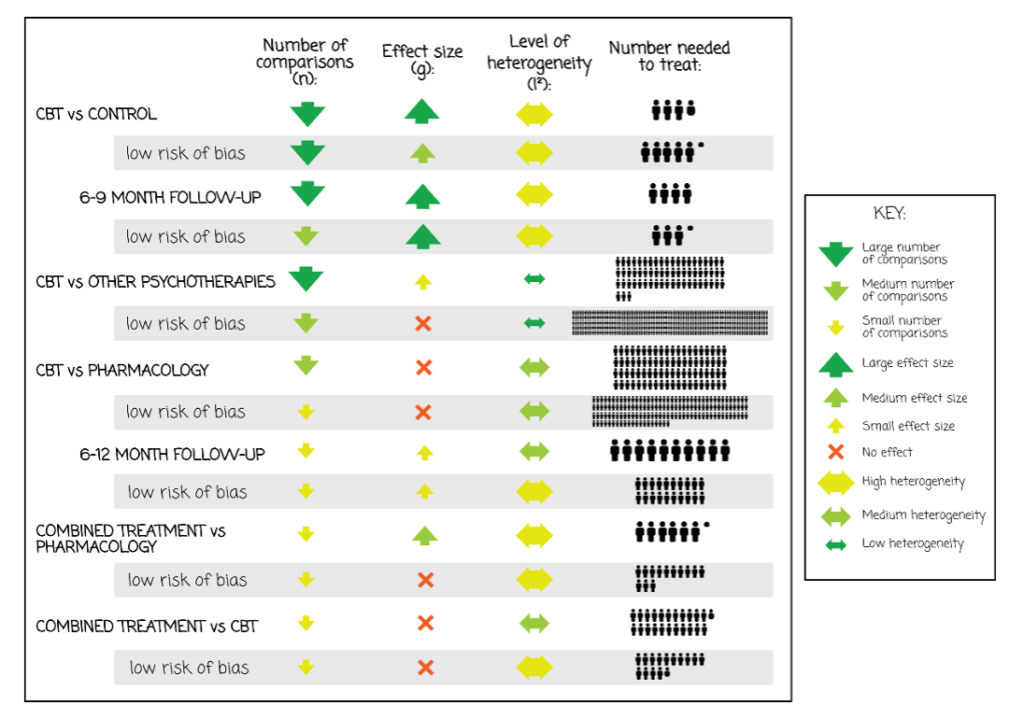
Many studies compared CBT to control conditions (n=271), with a large effect size (g=0.79, 95% CI: 0.70 to 0.89) indicating CBT is more effective than control conditions. With only a low risk of bias studies (n=9), the effect size is significantly lower (p=<0.001) but was still a medium effect size. However, across both comparisons, there was a high level of heterogeneity suggesting there is considerable variability between the studies.
At 6-9 months post-CBT, the effect size was found to remain high indicating the CBT was still more effective than controls half a year post-intervention (n=78, g=0.74, 95% CI: 0.36 to 1.11). A low risk of bias studies was reported (n=29, g=0.91, 95% CI: 0.46 to 1.36), though it is worth noting an increased heterogeneity, suggesting the variability between trials also rises with the increased effect. Further follow-up analysis sees a drop in effect sizes.
Compared to other psychotherapies, a small significant effect was found in favour of CBT (n= 87, g=0.06; 95% CI: 0 to 0.12; NNT=63) with low heterogeneity. Comparison of CBT to individual psychotherapies (e.g., supportive therapy, behavioural activation) did not indicate that CBT was any more effective. CBT was not found to be improved compared to pharmacology immediately post-intervention, but at 6-12 months a small significant effect indicated CBT was more effective than pharmacology.
Nonetheless, a combination of psychotherapies was compared to pharmacology treatment and indicated that combined treatment was more effective. Combined treatment compared to CBT alone was not significantly more effective. Across all these comparisons, heterogeneity was high.
Unguided CBT was found to have a small effect on reducing depression, upheld albeit with a lower effect size, with only a low risk of bias analyses. Both analyses had high and moderate heterogeneity respectively. Lastly, CBT was found to be more effective than control conditions with children and adolescents with a medium effect, yet high heterogeneity suggests increased variability between trials.
“The effectiveness of CBT for depression is documented across different formats, ages, target groups, and settings”. View full size image.
Conclusions
The authors concluded:
The efficacy of CBT in depression is documented across different formats, ages, target groups, and settings. However, the superiority of CBT over other psychotherapies for depression does not emerge clearly from this meta-analysis. CBT appears to be as effective as pharmacotherapies at the short term, but more effective at the longer term.
It is important to note that although CBT results in better response rates than control groups do, less than half of people find receiving CBT are classified as ‘responders’ and only about a third as ‘remitted’ from depression, so there is still considerable room for improving treatment outcomes and for better establishing what works for whom.

The findings further highlight the need to improve treatment outcomes for people with depression.
Strengths and limitations
The authors are very experienced in conducting systematic reviews and meta-analyses and leveraged their ongoing project on psychological treatments for depression to conduct this review. This study is incredibly impressive in its sheer volume of trials included, and comparisons made. It is perhaps second only to the Cipriani 2018 review on antidepressants for depression, as one of the largest ever meta-analyses of a specific type of therapy for a targeted mental health problem. The method for the meta-analytic project is openly accessible allowing reproducibility. The risk of bias in each of the included trials is systematically considered using the Cochrane Collaboration’s Risk of Bias tool, while the random effects model as the statistical approach used to pool the findings across studies was particularly robust to handle the data.
That said, this review doesn’t include publications from 2022 onwards, and using Hedges’ G as an effect size metric across studies makes an implicit assumption that all measures of depression used across the trials were equally good at detecting change. This is not likely to be the case, with some measures doing better than others and dependent on the population under investigation.
The authors themselves also note that the included studies were very diverse highlighted by the heterogeneity in the data, which creates caution about how this data should be interpreted and may make it less meaningful to pool the findings of each study statistically. Many of the included studies were judged to be at high risk of bias, and those that were at low risk of bias were less likely to have found large effects.
And as the authors searched for published papers, publication bias may mean that there are some trials with less favourable findings that aren’t included because they have never been published. The authors did try to mitigate this by correcting for this bias.

This is one of largest meta-analyses ever published on a specific type of psychological therapy for depression.
Implications for practice
It is really encouraging that CBT performs better than control conditions for reducing depression symptoms up to 12 months later and across many different formats and populations. CBT has been well tested for depression, and whilst there is still much room for improvement (e.g., the effect sizes are much more modest for child and adolescent trials than for trials in adults), we can be reasonably confident, given these findings, that CBT is worth investing in as a treatment approach. That said, one size doesn’t fit all, and again, it is encouraging that self-help CBT, even without human support input, was at least moderately good at reducing depression symptoms. This is implied by the heterogeneous findings, which could be further explored with subgroup analysis. With that in mind, we would like to see more attention given to what works for whom, and to making sure that people who are struggling with depression get choices, and information about how good (or not) each of these options are, based on the evidence, so that they can make an informed decision about what they want.
It does feel important though, to acknowledge here that many people with depression do not receive evidence-based therapy or any mental health support at all. Partly, systemic barriers such as lack of resources and training may disproportionately affect those living in more deprived conditions and in low- and middle-income countries. Moreover, interpersonal and within-person barriers like stigma and fear, or lack of knowledge may play a role too. Unfortunately, in cases where people access help, they may not have a choice about what that is or the delivery format – and that needs to change!

Offering CBT for depression is likely to be more effective than receiving other psychotherapies or no treatment.
Statement of interests
Dr Maria Loades is qualified in delivering Cognitive Behavioural Therapy and supervision, while her research interests include developing and delivering scalable CBT treatments for children and young people.
Links
Primary paper
Cuijpers, P., Miguel, C., Harrer, M., Plessen, C. Y., Ciharova, M., Ebert, D., & Karyotaki, E. (2023). Cognitive behavior therapy vs. control conditions, other psychotherapies, pharmacotherapies and combined treatment for depression: A comprehensive meta‐analysis including 409 trials with 52,702 patients. World Psychiatry, 22(1), 105–115.
Other references
Lee, Y., Stockings, E., Harris, M., Doi, S., Page, I., Davidson, S., & Barendregt, J. (2019). The risk of developing major depression among individuals with subthreshold depression: A systematic review and meta-analysis of longitudinal cohort studies. Psychological Medicine, 49(1), 92-102. doi:10.1017/S0033291718000557
Chisholm, D., Sweeny, K., Sheehan, P., Rasmussen, B., Smit, F., Cuijpers, P., & Saxena, S. (2016). Scaling-up treatment of depression and anxiety: A global return on investment analysis. The Lancet Psychiatry, 3(5), 415–424.
Zhang, R., Peng, X., Song, X., Long, J., Wang, C., Zhang, C., . . . Lee, T. (2022). The prevalence and risk of developing major depression among individuals with subthreshold depression in the general population. Psychological Medicine, 1-10. doi:10.1017/S0033291722000241
Photo credits
The photos in the Results section have been created by Camilla Babbage for the purposes of this blog.
