Oral lichen planus is a chronic or recurrent inflammatory autoimmune disease of the oral mucosa, typically characterized by the presence of white lace-like lesions, with or without atrophic or erosive areas. Patients typically complain of oral burning soreness or pain which impacts on eating, drinking and talking. The prevalence of oral lichen planus is estimated to be aroung 2% of the general population.
The aim of this review was to precisely estimate the global prevalence of oral lichen planus (OLP).
Methods
Searches were conducted in the PubMed, EMBASE, Web of Science, and Scopus databases. English language studies assessing oral lichen planus prevalence were considered. Where studies had reported in the same study population the most recently reported or those providing more data were included. Two reviewers selected studies and extracted data independently. Study quality was assessed using the Joanna Briggs Institute methods for systematic reviews of disease prevalence. Oral lichen planus prevalence data was extracted from studies and reported as proportions with 95% confidence intervals (CI). Random effect meta-analysis was conducted. Associations with sex, age, tobacco, and alcohol use were explored. And presented as odds ratios (OR) with 95%CI. Sensitivity analyses were performed to test the reliability of pooled results.
Results
- 66 observational studies (60 cross-sectional) were included involving a total of 500,464 patients of whom 5,392 were diagnosed with OLP.
- Study sample sizes ranged from 308 to 57,518.
- 21 were conducted in Asia, Europe 19, India 15, Central & South America 6, North America 4, and 1 in Africa.
- Diagnostic criteria were varied with 28 studies not explicitly defining criteria.
- Meta-analyses of the data with global and regional data are shown in the table below.
| Prevalence | No. of studies | No of patients | Prevalence (95%CI) |
| Global * | 71 | 500,464 | 1.01% (0.74 to 1.32%) |
| Africa | 1 | 4,470 | 1.43% (1.12 to 1.82%) |
| Asia (ex-India) | 26 | 84,489 | 1.08% (0.64 to 1.63%) |
| India | 15 | 218,490 | 0.49% (0.29 to 0.74%) |
| Europe | 19 | 90,692 | 1.32% (0.74 to 2.05%) |
| North America | 4 | 45,693 | 0.47% (0.13 to 1.02%) |
| South & Central America | 6 | 56,630 | 1.74% (0.13 to 5.09%) |
*66 studies were included, but data from the Asian Betel Quid consortium was meta-analysed as 6 different units.
- Meta-analysis showed that patents aged over 40 had increased odds of developing OLP; OR = 3.43 (95%CI;2.48 – 4.73).
- Buccal mucosa was the most common site for OLP.
| Lesion location | Prevalence (95%CI) |
| Buccal mucosa | 67.15% (58.79 to 75.02%) |
| Tongue | 10.47% (5.88 to 16.09%) |
| Gingivae | 7.26% (4.41 to 10.67%) |
| Lips | 5.59% (2.73 to 9.24%) |
| Palate | 2.22% (0.63 to 4.50% |
| Retromolar trigone | 0.25% (0.00 to 1.46%) |
| Floor of Mouth | 0.13% (0.00 to 0.67%) |
Conclusions
The authors concluded: –
our systematic review and meta-analysis revealed a global OLP prevalence of 1.01%, with marked geographical differences. The most robust results indicate that the highest prevalence appears in Europe (1.43%) and the lowest is in India (0.49%), where tobacco consumption may mask the detection of OLP. From the age of 40y., the prevalence of OLP increases significantly and progressively. Studies that define their diagnostic criteria have significantly higher OLP prevalence, although the use of the WHO criteria does not increase the ability to diagnose the disease compared to other criteria. We believe that reliable criteria should be defined, which should include the presence of white reticular lesions in any location of the oral mucosa.
Comments
This large well conducted meta-analysis included 66 studies the majority (90%) of which were cross-sectional in nature. As only English language studies were included there is the possibility that relevant studies were excluded although the authors do not that during piloting of the search strategy a number of potential eligible papers were duplicated in English. Another potential issue relates to the inclusion of 28 studies where the diagnostic criteria were not defined in detail or explicitly. With a range of different diagnostic criteria being employed in the included studies there is a need for an international consensus to agree reliable diagnostic criteria for future use.
Links
Primary Paper
González-Moles MÁ, Warnakulasuriya S, González-Ruiz I, et al. Worldwide prevalence of oral lichen planus: A systematic review and meta-analysis [published online ahead of print, 2020 Mar 7]. Oral Dis. 2020;10.1111/odi.13323. doi:10.1111/odi.13323
Other references
Dental Elf – 8th Aug 2018
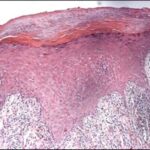
Picture Credits
By Shi G, Sohn KC, Choi DK, Kim YJ, Kim SJ, Ou BS, Piao YJ, Lee YH, Yoon TJ, Lee Y, Seo YJ, Kim CD, Lee JH – (2010). “Brn2 Is a Transcription Factor Regulating Keratinocyte Differentiation with a Possible Role in the Pathogenesis of Lichen Planus”. PLoS ONE 5 (10): e13216. DOI:10.1371/journal.pone.0013216. ISSN 1932-6203.CC BY 4.0, CC BY 4.0, Link
