
We know the stats. People with psychosis die younger, the mortality gap is not improving, and most people with psychosis die from chronic physical illness (Saha S. et al., 2007).
We also know that family carers play a critical role in managing our patients’ illness and maintaining their wellbeing. Family support is associated with improved engagement with treatment, reduced rates of relapse, as well as reduced mortality rates (Onwumere et al, 2019).
In the current viewpoint piece, Onwumere and colleagues (2019) put the two together and argue that family carers’ views should be considered in tackling the physical health problems in people with psychosis.

Family carers involvement plays a critical role in supporting patients.
Methods
In this article, the authors considered the following three main issues in turn before arriving at their concluding statement:
- Caregiving and patient physical health
- Family carer and patient health
- Recommendations for improving physical health outcomes in people with psychosis by supporting the roles of family carers.
Results
In examining the existing evidence for caregiving and patient physical health, the authors highlighted that:
- Family carers are exposed to a wide range of physical health conditions when caring for their relative with psychosis
- Family carers often struggle with discussing lifestyle modifications such as smoking, diet, and physical activity; not necessarily due to the lack of knowledge, but often in the context of a more subtle and complex prioritisation of their relative’s needs
- Only a limited number of studies have explored the perspective of family carers on this topic.
In terms of family carer and patient health, the authors remind us that being a family carer is associated with increased risk of poorer physical health including hypertension and diabetes.
Given these, the authors present the following recommendations to support the role of family carers:
- Recognise the role, knowledge, and expertise of family carers, as well as their needs for information and support regarding physical health problems
- Provide education about physical health from the onset of mental illness
- Provide specific guidance on how to communicate sensitive health issues with their family members (given the potential impacts of psychosis), as well as guidance on practical strategies that can be implemented easily to improve physical health
- Build greater awareness of the research underpinning the global focus on reducing physical health problems in people with psychosis, as part of building more hopeful dialogue on this issue
- Implement strategies that promote a focus on family carers looking after their own physical health and wellbeing.

Being a family carer is associated with an increased risk of poorer physical health status.
Conclusions
In summing up, the authors argue that:
- Family carers are often providing the bulk of care and are therefore important figures in a patient’s social network
- They are uniquely placed in the person’s immediate environment and therefore can impact their lifestyle and overall wellbeing
- Their perspective should therefore be sought on discussions and strategies to develop and implement lifestyle interventions
- Family carers want holistic and integrated approaches to the patient wellbeing.
They conclude that:
We have reached a stage where a more detailed understanding of carer needs, specifically as they relate to physical comorbidities in patients and their contributions to improving outcomes, are required.

Family carers are important figures in a patient’s social network.
Strengths and limitations
It is hard to argue against the passion and the common sense that are evident throughout this article. There are often two important aspects of care provision that seem to disappear in the overstretched, burnt-out mental health services (a cynic may read this as “treatment as usual”). Such services are often too focused on the diagnosis and overlook the social context in which the person with the diagnosis lives their life.
There is, however, an inherent difficulty in building a scientifically sound evidence base using passion and common sense. Could we randomly allocate a family carer to one group and a professional carer to another to see which type of care does better? It would not get through the ethics committee. Could we blindly follow the evidence from the cohort studies and accept that having a family carer is better than not having one? How about all the unadjusted confounders? Could we trust the saturation point in qualitative studies when we know clinically that family carer experiences are very heterogeneous, especially when such conclusions are built upon stories of a small number of self-selected family carers? In other words, some may argue that these recommendations and the conclusion are based on “fluffy” evidence.
Others would argue that randomised controlled trials (RCTs) are not good at measuring complexity (Greenhalgh et al, 2016). Like the fragmented health services that they examine, they are prone to taking siloed slices of the picture (the parts) and miss measuring and understanding the interlinked nature of human existence and service systems (the whole). This is especially so when the person experiences multi-morbidity that relies on good old communication across systems.
People’s experiences of lifestyle behaviour change and engagement with health services are equally heterogeneous. People are more than the tasks, actions and interventions dished out by health professionals or measured in research trials. That’s why we have seen an increasing focus on mixed methods research: quantitative methods tell us what is going on but we need qualitative research to help us understand why; the nuanced human experience.

Quantitative methods tell us what is going on but we need qualitative research to help us understand why.
Implications for practice
One of the most astute criticisms of this field was beautifully summarised in the title of an editorial: “so many publications, so little change” (Stewart 2015). Most of us clinicians do not need published articles to appreciate the importance of family carers in our patients’ lives. Many of us have chosen psychiatry because we wanted to help people. Can we trust our common sense, and invite family carers into our consultation rooms? Instead of giving clichéd tag-lines (e.g. “you should try to take 10,000 steps a day”), maybe we can talk about what the patient wants to do, what they may have already tried or are already doing, what they think would work, what we want the patient to do, and how we may be able to meet halfway with the resources and options that we have, and, where it’s OK to do so, include the family carer in the plan.
We should remind ourselves that living alongside the person is what family carers do and this gives them unique opportunities ‘in the moments’ to encourage, prompt, help the person problem-solve, follow through and help the person apply lifestyle knowledge and advice and adapt it to their specific circumstances and preferences. Family carers are good problem-solvers and system navigators, stoic and persistent, or they must quickly become so because of the often fragmented service systems that they experience as part of their caring role.
And please, please, let us not label the process anything fancy. Let us change the way we justify what we do. Listening to the patient and having their family carer in the room should be part of what we do day to day, consultation after consultation (just like the good ol’ days, some may say). It should be called psychiatry, not motivational interviewing, psychoeducation, or family intervention.
“So many publications, so little change”.
Conflicts of interest
None.
Links
Primary paper
Onwumere J, Shiers D, and Gaughran F. (2019) Physical Health Problems in Psychosis: Is It Time to Consider the Views of Family Carers? Frontiers in Psychiatry 2019 9:668.
Other references
Greenhalgh T, Annadale E, Ashcroft R, et al (2016) An open letter to the BMJ editors on qualitative research. British Medical Journal 2016 10; 352:i563
Lawn S, McNaughton D, and Fuller L. What carers of family members with mental illness say, think and do about their relative’s smoking and the implications for health promotion and service delivery: a qualitative study. International Journal of Mental Health Promotion 2015 17 (5) 261 – 277. [Abstract]
Saha S, Chant D, and McGrath J. (2007) A systematic review of mortality in schizophrenia: Is the differential mortality gap worsening over time? Archive of General Psychiatry 2007 64(10) 1123 -1131. [PubMed abstract]
Stewart K. (2015) Mental disorders and mortality: so many publications, so little change. Acta Psychiatrica Scandinavica 2015 132 (5) 410 – 411.
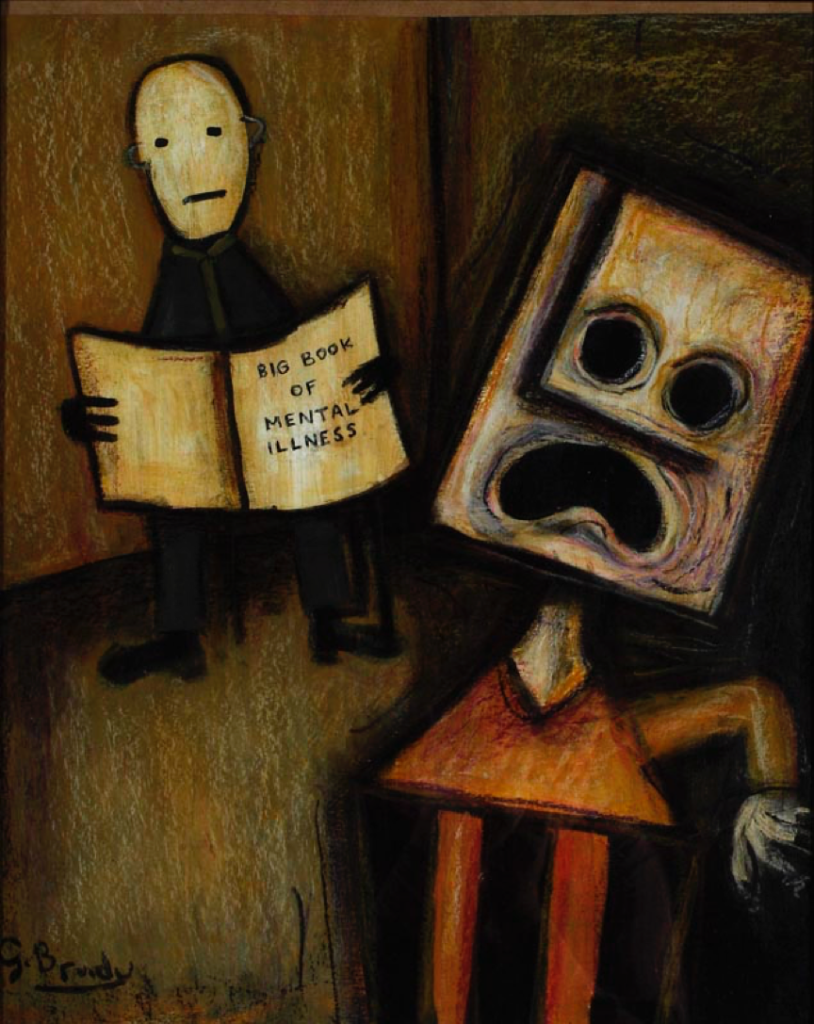
Photo credits
All images are from Queensland Centre for Mental Health Research gallery.
