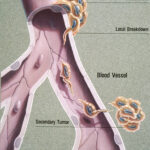
Oral cancer is a global major health burden (Dental Elf – 16th October 2020) being the eight common cancer worldwide with incidence ranging from 1 to 10 cases per 100,000 population in many countries, with squamous cell carcinoma the most common type (Dental Elf – 29th June 2020). The incidence of oral cancer is more common in developing countries (compared to developed countries) especially in South-Central Asia, where cancer of the oral cavity is among the three most common types of cancer (Petersen 2009). Metastatic tumours to the oral and maxillofacial regions are reported to account for 1% of all oral and maxillofacial malignancies. There are clinical challenges in diagnosing a metastasis which can resemble benign inflammatory and hyperplastic lesions. The aim of this systematic review was to summarise the available information around metastasis to the oral and maxillofacial region.
Methods
The Preferred Reporting Items for Systematic Review and Meta-Analyses were used to inform the methodology of this review. PubMed, Web of Science, Scopus, Embase and LILACS were the databases searched. Additionally, there were manual searches performed of references of included articles. The criteria for metastasis were adapted from Calusen and Poulsen (1963) for the inclusion criteria. Only primary studies were included, experimental conditions were excluded. Studies were included if they assessed the potential diagnostic value or other discriminatory properties of biological markers in the saliva of patients with COVID-19.
Results
- 3349 articles were retrieved across the initial database search. Following removal of duplicates and implementation of the inclusion and exclusion criteria, 217 studies were included in the review. This includes 190 case reports and 24 case series giving a total of 348 cases.
- The studies were published across a number of countries. The cases were more prevalent among males than females (males: n=199; 57.68% vs females: 146; 42.32%), the mean age of diagnosis was 58.29 years (+/- 15.8) ranging from 8 months to 90 years.
- Regarding anatomical location of the metastasis, bone tissue (n=183; 53.19%) was more affected than soft tissue (n=140; 40.69%) and multiple sites affected in 21 patients (6.10%). For bone tissue, the mandible (n=144; 41.86%) was more affected than the maxilla (n=26; 7.55%). For soft tissue, lesions in the gingiva were more prevalent (n=80; 23.25%), followed by the tongue (n=23; 6.68%) and parotid gland (n=14; 4.09%).
- 109 patients (60.56%) reported pain whilst 71 patients (39.44%) had no pain. The most prevalent clinical presentation was a nodule (n=280; 85.89%) and some were associated with ulceration (27.14%) or paraesthesia (14.64%).
- In 203 patients (70%), the primary site was diagnosed before the metastatic site while in 87 patients (30%), the metastatic site was discovered first.
- There were a range of 29 primary sites, the most affected being the lungs (n=73; 20.97%), breast (n=42; 12.06%) and kidney (n=41; 11.78%).
- The overall 3-year and 5-year survival rates were 17.7% and 7.3% respectively.
Conclusions
The authors concluded: –
…oral metastasis are uncommon and challenging for the clinician.
Comments
This systematic review extracts a number of parameters from included studies that highlight common findings of metastasis to the oral and maxillofacial regions. There was no quality assessment of included studies or any statistical calculations however the authors did report this was a study of case reports and case series, hence heterogeneity of such studies can preclude quantitative analysis. The frequency of developing oral and maxillofacial metastasis differs depending on the primary cancer organ site which is useful information for screening to identify the primary site if unknown. Whilst this systematic review is informative and an important reminder for clinicians to be vigilant for metastasis in the oral and maxillofacial region, no change in clinical practice is recommended.
Links
Primary paper
Other references
Clausen F, Poulsen H. Metastatic carcinoma of the jaws. Acta Pathol Microbiol Scand. 1963;57:361-74. doi: 10.1111/j.1699-0463.1963.tb05105.x. PMID: 14064805.
Petersen PE. Oral cancer prevention and control–the approach of the World Health Organization. Oral Oncol. 2009 Apr-May;45(4-5):454-60. doi: 10.1016/j.oraloncology.2008.05.023. PMID: 18804412.
Shen ML, Kang J, Wen YL, Ying WM, Yi J, Hua CG, Tang XF, Wen YM. Metastatic tumors to the oral and maxillofacial region: a retrospective study of 19 cases in West China and review of the Chinese and English literature. J Oral Maxillofac Surg. 2009 Apr;67(4):718-37. doi: 10.1016/j.joms.2008.06.032.PMID: 19304027.
Dental Elf – 29th June 2020
Elective neck dissection versus observation for T1-2 oral squamous cell carcinoma
Dental Elf – 16th October 2020
Optical fluorescence imaging in oral cancer and potentially malignant disorders
Picture Credits
By Jane Hurd (Illustrator) – This image was released by the National Cancer Institute, an agency part of the National Institutes of Health, with the ID 2446 (image) (next)., Public Domain,
