
Last year, the Washington Post featured a “Medical Mysteries” column that described a 23-year-old woman with episodes of what seemed like mania and psychosis that led to a 6-month stint in a residential treatment program (Boodman, 2022). When her symptoms failed to respond to medications and she began to have trouble walking, she was to be admitted to a psychiatric hospital for intensive care. While en route however, an ER doctor decided to order computerised tomography (CT) of her head and, low and behold, she was found to have “the most severe case of hydrocephalus” the doctor had ever seen. Needless to say, the psychiatric admission was called off and the patient instead underwent a surgical ventriculostomy that resulted in a drastic improvement, if not complete resolution, of her psychiatric symptoms.
Although such cases suggest that everyone with first-episode psychosis (FEP) should receive neuroimaging so that an “organic” cause of psychosis isn’t missed, the clinical yield and cost-effectiveness of such screening has long been debated. While some guidelines have recommended routine screening (Gallety et al., 2016), a systematic review concluded that “little would be found to affect clinical management” if structural neuroimaging were performed routinely in people with new onset psychosis who are under 65 years old (Albon et al., 2008). Forbes and colleagues (2019) likewise concluded that there is “insufficient evidence to suggest that brain imaging should be routinely ordered for patients presenting with [FEP] without associated neurological or cognitive impairment”.
While several studies have been conducted through the years to assess the clinical utility of neuroimaging in FEP, the results have been inconsistent. For example, Williams et al. (2014) found no neuroimaging abnormalities in a sample of 115 patients with FEP. However, another study examined findings from brain magnetic resonance imaging (MRI) obtained for research purposes among patients with FEP and found that 30% had abnormal scans (Lubman et al., 2002), whilst elsewhere it has been reported that 64% of those with FEP had brain lesions detected by either CT or MRI (Khandanpour et al., 2013). However, in the vast majority of cases, such abnormalities were deemed to represent incidental findings unrelated to psychosis and not requiring urgent care. To add to the inconsistency of these results, some studies using healthy controls for comparison have reported a greater incidence of neuroimaging abnormalities among those with psychosis spectrum illness (Borgwardt et al., 2006; Khandanpour et al., 2013;), while others have found no difference (Lubman et al., 2002; Zanetti et al., 2008; Sommer et al. 2013).
Several outstanding questions are, therefore, relevant to the clinical utility of neuroimaging in first episode psychosis (FEP):
- What is the true rate of brain abnormalities detected by neuroimaging in FEP?
- Is the rate of neuroimaging abnormalities in FEP significantly different from healthy controls?
- What types of brain abnormalities are detected and are they clinically significant as causal explanations for psychosis?
In order to address the heterogeneity of outcomes to date, Blackman et al. (2023) have recently published a systematic review and meta-analysis of studies examining neuroimaging abnormalities in patients with FEP. Will it finally give us some answers to these key questions about the clinical utility of neuroimaging in FEP? Let’s find out.

To date, neuroimaging studies have yielded inconsistent findings about the rate of brain abnormalities in first episode psychosis and their clinical relevance.
Methods
The authors narrowed 1,682 publications down to 12 studies reporting the frequency of intracranial abnormalities as detected by MRI among patients with FEP published between 1991 and 2022. These studies involved 1,613 patients with FEP with no overlapping samples. Five studies reported data from routine clinical practice, while 6 reported data from clinical research studies. Eight studies included a healthy control group and 10 excluded patients in whom a potential secondary cause of psychosis was suspected prior to neuroimaging. Nine studies reported on the clinical relevance of detected abnormalities, where clinical relevance was defined by the meta-analysis authors as resulting in a change in management or diagnosis, including referral to a medical specialty.
For each study, the proportion of FEP patients with a neuroimaging abnormality was calculated with 95% confidence intervals. Risk ratios were calculated to compare rates of intracranial abnormalities between FEP patients and healthy controls.
Neuroimaging abnormalities were categorised as white matter, vascular, ventricular, cyst, pituitary tumor, cerebral atrophy, and “other.” To assess the clinical utility of neuroimaging, the estimated number of patients needed to be scanned to detect 1 abnormality (number needed to assess [NNA]) was calculated based on the reciprocal of the prevalence estimate. Statistical analyses were also performed to examine for study bias and heterogeneity with a sensitivity analysis performed to determine the effects of excluding studies with a mean patient age > 35, studies in which assessments were performed by a non-radiologist, and studies based on research as opposed to clinical samples.
Results
The sample size ranged from 20 to 349 patients across the 12 studies with a mean age range of 20 to 60 years. Duration of psychosis ranged from 4 to 52 weeks with 65% of the total sample receiving antipsychotic medication.
The pooled prevalence of radiological abnormalities among those with FEP was 26.4% (95% CI, 16.3 to 37.9%) while the pooled prevalence of clinically relevant abnormalities was 5.9% (95% CI, 3.2 to 9.0%). The most common radiological findings involved white matter abnormalities (e.g., mostly small hyperintensities) in 8% of patients followed by ventricular abnormalities in 5%. For clinically significant abnormalities, 0.9% had white matter hyperintensities and 0.5% had cysts.
Compared to healthy controls, the relative risk of any intracranial abnormality was 2.8 (95% CI, 1.3 to 5.9) and 1.5 (95% CI, 0.8 to 2.8) for clinically relevant abnormalities.
The number needed to assess (NNA) was 4 for any radiological abnormality and 18 for clinically relevant abnormalities.
Statistical analysis found a high degree of heterogeneity, but no clear evidence of publication bias. Sensitivity analyses demonstrated no effects of age, assessment by a non-radiologist, or research samples on the significance of pooled estimates.

Intracranial abnormalities were present in over a quarter of patients with FEP and were nearly 3 times more frequent compared to healthy controls.
Conclusions
While the rate of intracranial abnormalities detected by MRI was 26%, the rate of abnormalities judged to be clinically significant was only 6% with a risk ratio of 1.5 relative to healthy controls.
The rate of neuroimaging findings that result in diagnostic revision or referral to a specialist—but not necessarily a change in treatment—is much lower.
Strengths and limitations
Compared to previous systematic reviews of neuroradiologic findings in patients with FEP (Goulet et al., 2009; Forbes et al. 2019), this new meta-analysis includes studies published through 2022, but limited its scope to only studies utilising brain MRI. The exclusion of studies using CT was justified by noting that previous studies using CT have found substantially lower rates of intracranial abnormalities, suggesting a failure to detect them. As a result, the reported prevalence of neuroradiological abnormalities in this study would be expected to be greater than other studies including CT.
The authors’ definition of clinical relevance as leading to a change in management including merely referring a patient to a medical specialty limits any conclusions about clinical utility with regard to the management of psychosis. Consistent with previous studies, the rate of neuroimaging findings representing a potential cause of psychosis—that is, a change in diagnosis to a non-psychiatric disorder with a non-psychiatric intervention—was negligible.
However, since 10 of the 12 studies included in the meta-analysis excluded patients with clinical suspicion of a secondary cause of psychosis prior to neuroimaging, the rate of clinically relevant intracranial abnormalities detected by routinely neuroimaging patients with FEP in clinical practice could be substantially higher.
The authors did not or were not able to compare the rate of neuroimaging abnormalities between the 65% of patients with FEP who were receiving medication to those that were not. Unfortunately, this precludes any conclusions about possible medication effects. The meta-analysis also did not allow for any examination of potential harms of neuroimaging (e.g., radiation exposure from CT scanning, claustrophobia from MRI) or a cost-effectiveness analysis based on economic burden.

The authors did not consider the potential harms of neuroimaging, such as radiation exposure from CT or claustrophobia from MRI scanning.
Implications for practice
Based on a number needed to assess (NNA) of 18 for clinically relevant abnormalities, Blackman et al. (2023) conclude that their findings “support the use of MRI as part of the initial clinical assessment of all patients with FEP.” However, due to the authors’ liberal definition of clinical relevance together with the exclusion of patients with a suspected non-psychiatric cause of psychosis in most of the included studies, it remains debatable whether routine screening is warranted for all patients with FEP. Given recent evidence about the prevalence of autoimmune encephalitis as a potential cause of FEP (Scott et al., 2018), there may be other diagnostic procedures that are better warranted than routine neuroimaging in FEP depending on clinical presentation.
It could be argued that the clinical utility and risk:benefit ratio of neuroimaging ultimately boils down to cost. If neuroimaging were quick, easy, safe, and cheap—like an electrocardiogram (ECG) for the work-up of chest pain—then widespread neuroimaging for all cases of FEP would be more justifiable. Since it is not, it remains reasonable to limit neuroimaging to cases where there is some other clinical reason, such as advanced age, to suspect a non-psychiatric cause of psychosis. Such case-by-case consideration is consistent with most existing treatment guidelines (Forbes et al., 2019).
In clinical practice, neuroimaging is typically ordered to rule out entities like a brain neoplasm or encephalitis due to infectious or inflammatory causes due to the presence of other neurological symptoms or signs including motor symptoms, seizures, or delirium. While it would be helpful to understand the clinical utility of that practice, the current meta-analysis does not address the clinical yield of neuroimaging when there is a suspected non-psychiatric cause of psychosis.
That said, psychosis is a neurological—that is, a brain-mediated—symptom. Accordingly, the use of neuroimaging to detect biological markers that might account for psychiatric causes of FEP, like schizophrenia, remains a worthwhile goal of ongoing research. Indeed, data from half of the studies included in the meta-analysis were collected as a part of such research endeavours.
While the authors argue that the most common finding of white matter hyperintensities could reflect pathological processes relevant to psychosis and that such findings may predict subsequent morbidity later in life, the real-world clinical utility of such findings—often described as “unidentified bright objects” or “UBOs” is questionable.
Tantalising new research investigating neuroimaging findings in patients at high risk for psychosis suggests that the evolution of psychosis disorders like schizophrenia may be better accounted for by differences in grey and white matter volume or regional cortical thickness (ENIGMA Clinical High Risk for Psychosis Working Group 2021; Collins et al., 2022). Such subtle findings are not likely to be discernible in routine clinical neuroimaging and may depend on more sophisticated neuroimaging techniques.

Routine neuroimaging in FEP might reveal intracranial abnormalities but the vast majority would not be expected to provide a non-psychiatric explanation of psychosis resulting in a significant change in treatment approach.
Statement of interests
None.
Links
Primary paper
Blackman G, Neri G, Al-Doori O, Teixeira-Dias M, Mazumder A, Pollak TA, Hird EJ, Koutsouleris N, Bell V, Kempton MJ, McGuire P. Prevalence of neuroradiological abnormalities in first-episode psychosis: A systematic review and meta-analysis. JAMA Psychiatry 2023; 80:1047-1054.
Other references
Albon E, Tsourapas A, Frew E, Davenport C, Oyebode F, Bayliss S, Arvantis T, Meads C. Structural neuroimaging in psychosis: A systematic review and economic evaluation. Health Technology Assessment 2008; 12:18.
Andreou C, Borgwardt S. Structural and functional imaging markers for susceptibility to psychosis. Molecular Psychiatry2020; 25:2773-2785.
Boodman SG. She was headed to a locked psych ward. Then an ER doctor made a startling discovery. The Washington Post; February 12, 2022.
Borgwardt SJ, Radue E-W, Götz K, Aston J, Drewe M, Gschwandtner U, Haller S, Pflüger M, Stieglitz R-D, McGuire PK, Riecher-Rössler A. Radiological findings in individuals at high risk of psychosis. Journal of Neurology, Neurosurgery, and Psychiatry 2006; 77:229-233.
Collins, MA, Li JL, Chung Y, Lympus CA, Afriyie-Agyemang Y, Addington JM, Goodyear BG, Bearden CE, Cadenhead KS, Mirzakhanian H, Tsuang MT, Cornblatt BA, Carrion RE< Keshevan M, Stone WS, Mathalon DH, Perkins DO, Walker EF, Woods SW, Powers AR, Anticevic A, Cannon TD. Accelerated cortical thinning precedes and predicts conversion to psychosis: The NAPLS3 longitudinal study of youth at clinical high-risk. Molecular Psychiatry 2022; 28:1182-1189.
ENIGMA Clinical High Risk for Psychosis Working Group. Association of structural magnetic imaging measures with psychosis onset in individuals at clinical high risk for developing psychosis. JAMA Psychiatry 2021; 78:753-766.
Forbes M, Stefler D, Velakoulis D, Stuckey S, Trudel J-F, Eyre H, Boyd N, Kisely S. The clinical utility of structural neuroimaging in first-episode psychosis: A systematic review. Australian & New Zealand Journal of Psychiatry 2019; 53:1093-1104.
Galletly C, Castle D, Dark F, Humberstone V, Jablensky A, Killacky E, Kulkarni HJ, McGorry P, Nielssen O, Tran N. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the management of schizophrenia and related disorders. Australian and New Zealand Journal of Psychiatry 2016; 50:410-472.
Goulet K, Deschamps B, Evoy F, Trudel J-F. Use of brain imaging (computed tomography and magnetic resonance imaging) in first-episode psychosis: Review and retrospective study. The Canadian Journal of Psychiatry 2009; 54:493-501.
Khandanpour N, Hoggard N, Connolly DJA. The role of MRI and CT of brain in first-episodes of psychosis. Clinical Radiology 2013: 68:245-250.
Lubman DI, Velakoulis D, McGorry PD, Smith DJ, Brewer W, Stuart G, Desmond P, Tress B, Pantelis C. Incidental radiological findings on brain magnetic resonance imaging in first-episode and chronic schizophrenia. Acta Psychiatrica Scandinavica 2002; 106:331-336.
Scott JG, Gillis D, Ryan AE, Hargoven H, Gundarpi N, McKeon G, Hatherill S, Newman MP, Parry P, Prain K, Patterson S, Wong RCW, Wilson RJ, Blum S. The prevalence and treatment outcomes of antineuronal anti-body-positive patients admitted with first episode psychosis. BJPsych Open 2018; 4:69-74.
Sommer IE, de Kort GAP, Meijering AL, Dazzan P, Hulshoff Pol KE, Khan RS, van Haren NEM. How frequent are radiological abnormalities in patients with psychosis? A review of 1379 MRI scans. Schizophrenia Bulletin 2013; 39:815-819.
Zanetti MV, Schaulfelberger MS, de Castro CC, Menezes PR, Scazufca M, McGuire PK, Murray RM, Busatto GF. White-matter hyperintensities in first-episode psychosis. The British Journal of Psychiatry 2008; 193:25-30.
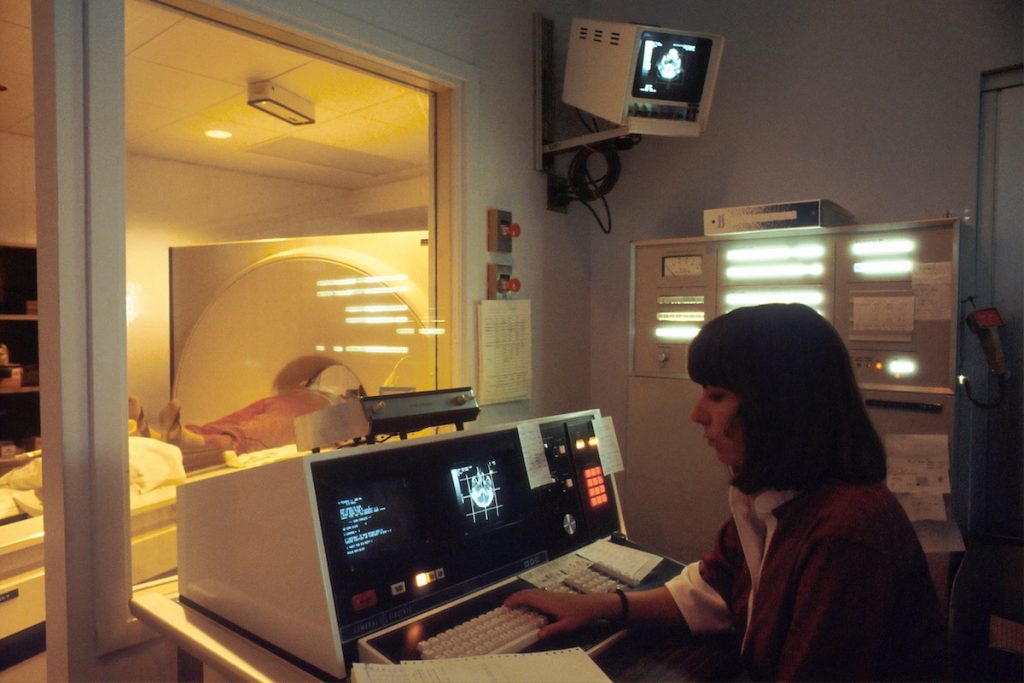
Photo credits
- Photo by National Cancer Institute on Unsplash
- Photo by Accuray on Unsplash
