
In recent times, few drugs have caused more excitement among clinical researchers than ketamine. It’s well known for its role in anaesthesia and veterinary surgery (“horse tranquilizer”), as well as its illicit use, but progress has been ongoing for about 15 years to repurpose it as an antidepressant.
As a consequence, many new studies are published every month that evaluate to what extent ketamine lives up to its promise as a new antidepressant drug (Aan Het Rot, Zarate, Charney, & Mathew, 2012). To make sense of the flood of new information, naturally intrigued mental elves clearly need researchers to provide timely updates of the current state of knowledge. To this end, Coyle and Laws (2015) have recently published an extensive systematic review and the first meta-analysis that summarises the latest, methodologically sound research.
The key questions of interest to these researchers were:
- Does ketamine have an immediate effect in reducing depressive symptoms?
- Are the antidepressant effects of ketamine sustained over time?
- Are repeat infusions more effective in reducing depressive symptoms?
- Do primary diagnosis and experimental design moderate the impact of ketamine on depressive symptoms?
- Do men and women experience differences in the antidepressant effect of ketamine?

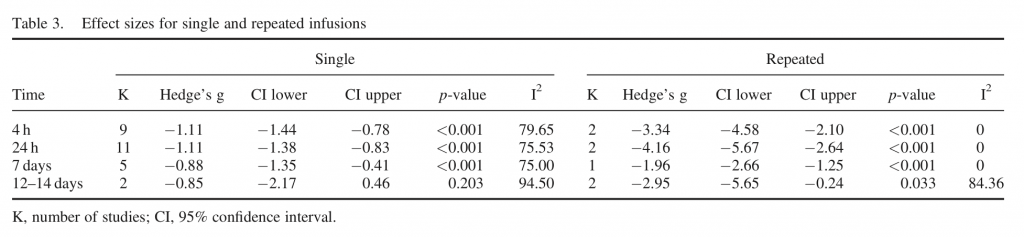
This review looked at how well the effects of ketamine are maintained over 4 hours, 24 hours, 7 days and 12-14 days.
Methods
The authors followed PRISMA guidelines and scanned all relevant medical databases for studies assessing the antidepressant potential of ketamine in patients with major depressive disorder (MDD) and bipolar disorder (BD). To evaluate possible methodological factors and design variables, the authors also specifically assessed whether studies were: repeat/single infusion, diagnosis, open-label/participant-blind infusion, pre-post/placebo-controlled design and patients’ sex.
Effect sizes were calculated either relative to placebo or relative to baseline, in case no control group was provided. To correct for bias in small studies, a Hedge’s g procedure with random effects was used. Statistical heterogeneity, publication bias and moderator variables were assessed to have an idea of other variables that might influence the reported antidepressant potential of ketamine. Statistical heterogeneity among studies was assessed using I² values, with values above 50% generally representing substantial heterogeneity.
Results
In total, 21 studies enrolling 437 patients receiving ketamine were identified that satisfied inclusion criteria:
- 17 were single infusion studies and the majority reported data collected at 4h (11) and 24h (13) after ketamine treatment
- 6 studies had follow-up for 7 days
- 4 studies had follow-up for 12-14 days
In general, there are grounds to assume publication bias for single infusion studies at 4h and 24h.
Of the 21 included studies, 2 were judged to be at a high risk of bias, 13 medium risk and 6 low risk of bias.
- In general, ketamine had a large statistical effect on depressive symptoms that was comparable across all time points
- Effect sizes were significantly larger for repeat than single infusion at 4 h, 24 h and 7 days
- For single infusion studies, effect sizes were large and significant at 4 h, 24 h and 7 days
- The overall pooled effect sizes for single and repeated ketamine infusions found no difference at any time point, suggesting that the antidepressant effects of ketamine are maintained for at least 12-14 days
Moderator analyses suggest that responsiveness to ketamine may vary according to diagnosis. Specifically, while ketamine produced moderate to large effects in both MDD and BD patients, the effect of a single infusion was significantly larger in MDD than BD after 24h. On the other hand, after 7 days, this pattern reversed and ketamine showed higher efficacy in BD patients. However, the small number of studies makes it tricky to draw any conclusions.
In addition, single-infusion pre-post comparisons did not differ in effect size estimation from placebo-controlled designs except for at 12-14 days, where only one study was available. In a similar vein, there were no effect size differences between single infusion studies with open-label and blinded infusions.
Of note, the meta-analysis found the percentage of males in the group was positively associated with ketamine’s antidepressant effects after 7 days, although this finding warrants replication with more data points.

There’s plenty of room for improvement in the primary research, but this meta-analysis shows ketamine in a promising light as an antidepressant.
Conclusions
The authors conclude:
Single ketamine infusions elicit a significant anti-depressant effect from 4h to 7days; the small number of studies at 12-14 days post infusion failed to reach significance. Results suggest a discrepancy in peak response time depending upon primary diagnosis – 24 h for MDD and 7 days for BD. The majority of published studies have used pre-post comparison; further placebo-controlled studies would help to clarify the effect of ketamine over time.
Limitations
This meta-analysis suffers from several limitations that are inherent in the available studies:
- For one, there were only four studies that assessed the effect of repeated ketamine infusions, which is a shame given that maintenance of antidepressant effects is one of the key drawbacks of rapidly acting interventions
- In addition, the authors note that their results suggest publication bias, which may be taken to indicate that several negative findings have not been published and thus could not be included in this meta-analysis
- Also, more information about adverse effects would have been useful, especially to evaluate whether ketamine can be safely applied in a broader clinical context
Summary
This is the first meta-analysis to evaluate ketamine’s antidepressant effects. For single infusion specifically, ketamine exerts large antidepressant effects in MDD as well as BD patients that seem to last at least 7 days, while too few studies are available beyond this time point.
It’s noteworthy that the effect sizes did not differ between time points, which indicates that the effect of a single infusion remains relatively stable in the short-term. While repeated infusions were shown to provide higher effects than single infusions at least for the first week, more studies are needed to corroborate the supremacy of repeated treatment.
Before ketamine can become a clinically viable treatment option, however, this review makes it clear that more methodologically refined studies (especially RCTs with adequate placebo controls) need to be conducted. With this in mind, researchers should take these findings as an incitement to action!

High quality placebo controlled trials are needed to drive forward progress in this field.
Links
Primary paper
and (2015), The use of ketamine as an antidepressant: a systematic review and meta-analysis. Hum. Psychopharmacol Clin Exp, doi: 10.1002/hup.2475. [PubMed abstract]
Other references
Aan Het Rot, M., Zarate, C. a, Charney, D. S., & Mathew, S. J. (2012). Ketamine for depression: where do we go from here? Biological Psychiatry, 72(7), 537–47. doi:10.1016/j.biopsych.2012.05.003


The antidepressant effects of ketamine are confirmed by a new systematic review and meta-analysis: Helge Hasse… http://t.co/vd24SEZeCz
RT @Mental_Elf: The antidepressant effects of ketamine are confirmed by a new systematic review and meta-analysis http://t.co/m9KDxNTe1D
The antidepressant effects of ketamine are confirmed by a new systematic… http://t.co/L6W2zFKUgQ #MentalHealth http://t.co/TPzlBnrrgP
Helen House liked this on Facebook.
Caroline Davis liked this on Facebook.
Raluca Lucacel liked this on Facebook.
Only shows there might be a positive effect much more research needs to be done. Very early days.
Mosaic Training Consultancy Ltd liked this on Facebook.
Denise Evangelista liked this on Facebook.
Andy Conway liked this on Facebook.
@Mental_Elf Confirmed? No way. Short term, no RCT, pub bias, etc. Plus nosologic doubts. Can’t help thinking of Pandora… @CoyneoftheRealm
@NabuccoDream @CoyneoftheRealm @Mental_Elf Pandora was an n=1 interventional case study, which reported multiple severe adverse events.
@TheLancetPsych @CoyneoftheRealm @Mental_Elf Haha! “How to destroy Greek Myths in 1 simple step.” I pretended to stress need for prudence.
@TheLancetPsych @CoyneoftheRealm @Mental_Elf Blog author’s description “he has a hunch that ketamine may be the next blockbuster drug”. COI?
@Mental_Elf “Researchers should take these findings as an incitement to action!” Hell no… Sciencie with conscience, please…
The antidepressant effects of ketamine – http://t.co/1nnG0bEii6
Michael Dalili liked this on Facebook.
Scott Inglis liked this on Facebook.
Don’t miss: New meta-analysis shows ketamine in a promising light as an antidepressant http://t.co/m9KDxOaPqd #EBP
@Mental_Elf – not rocket science but bad science -solution not in drugs- look at global spend on anti-depressants! @YoungMindsUK @rcpsych
@Mental_Elf Ketamine is a mood altering drug – young people become dependent – it’s been a significant problem #TimeToMind #substanceabuse
Mental Elf: The antidepressant effects of ketamine are confirmed by a new systematic review and meta-analysis http://t.co/HS6HTBbBob
The #antidepressant effects of #ketamine are confirmed by a new systematic review and meta-analysis http://t.co/jV18JkWH15 via @Mental_Elf
The antidepressant effects of ketamine are confirmed by a new systematic review and meta-analysis http://t.co/eSUkBIm02i via @sharethis
Interesting find- what do we think about this possibility?
http://t.co/qcJZiKienE
I’m never taking that ,
Most popular blog this week? It’s @Keith_Laws new SR on the antidepressant effects of #ketamine http://t.co/m9KDxOaPqd
@Mental_Elf @Keith_Laws – the horse tranquilliser? How apt for getting through in today’s society
[…] http://www.thementalelf.net/mental-health-conditions/depression/the-antidepressant-effects-of-ketami… […]
I have been depressed for years until I started to take ketamine.
[…] The antidepressant effects of ketamine are confirmed by a new systematic review and meta-analysis (10/04/15) […]
[…] Les hele artikkelen […]