
Mental health in the workplace is an area that we’ve blogged about a few times before. This blog features a recent review by Tan et al on workplace interventions for depression.
Mental disorders are the leading cause of sickness absence (Harvey, 2009 and Henderson, 2011), and depression in particular is predicted to be the leading cause of work disability by 2020 (Mathers, 2006). The significance of work to our mental health isn’t surprising considering we spend an average of 60% of our waking hours at work (WHO, 2008).
Although it is often said that prevention is better than cure, most workplace interventions are implemented reactively when an employee is already ill and on costly sick-leave. However, research on mental health interventions suggests they can result in a favourable return on investment (Hamberg-van Reenen, 2012). Employers may then be interested to see if preventative interventions result in a happier and more productive workforce.
Tan et al set out to systematically review and undertake a meta-analysis of randomised controlled trials (RCTs) of workplace prevention of depression. They were particularly interested in those programmes aimed at the universal workforce, not just those individuals at greater risk of depression.
Mental disorders are the leading cause of sickness absence worldwide, and depression is predicted to be the leading cause of work disability by 2020
Methods
An extensive search of electronic databases identified 17 RCTs of which nine were assessed to be of fair quality. For inclusion the studies needed to involve comparing a treatment group with a control group. Outcomes had to be measured using standardised self-report questionnaires both before and after intervention. The interventions needed to be aimed at the universal workforce, not just those at risk for depression. They also had to have a follow up period of at least four weeks.
The studies featured a range of interventions:
- Five were based on CBT including a range of techniques such as psycho-education, behavioural modification, stress management and acceptance and commitment therapy
- Two focused on mental health literacy
- One was based on exercise
- One centred on team-based participation to reduce stress in the workplace
- Most involved multiple sessions but one featured a single session of four hours
- All featured face-to-face interaction with the intervention facilitators
Results
Tan et al represented the effect size through standardised mean difference (SMD) that compares the outcome measures of depression in the treatment and control group after the intervention.
Here’s what they found:
- Overall the mean difference between intervention and control groups was 0.16 (95% Confidence Interval (CI) 0.07 to 0.24; p=0.0002)
- Effect sizes ranged from small negative effects (d=-0.01) to moderate positive effects (d=0.61)
- A separate analysis of only CBT based interventions showed an overall mean difference of 0.12 (95% CI 0.02 to 0.22; p=0.01)
- There was no evidence of significant publication bias

CBT came out best overall, but did this review cut the mustard?
Conclusions
The authors concluded that:
There is good quality evidence that universally delivered workplace mental health interventions can reduce the level of depression symptoms among workers. There is more evidence for the effectiveness of CBT-based programs than other interventions. Evidence-based workplace interventions should be a key component of efforts to prevent the development of depression among adults.
However, there are several limitations to the research that makes us think the authors’ conclusion is too optimistic.
Limitations
- Bias. None of the trials were blinded meaning participants knew if they were receiving the intervention or not. This means that a layer of expectation could cause participants to exaggerate reductions in their symptom scores – this is known as the Hawthorn effect.
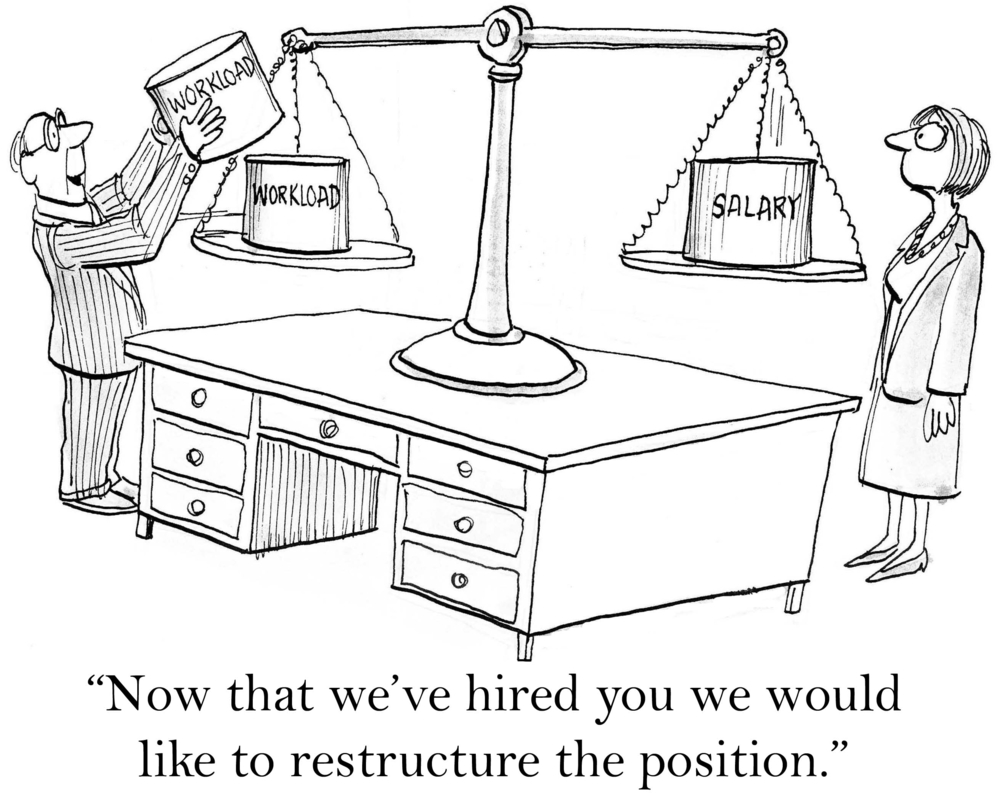
- What helped? In these RCTs the treatment group were given an intervention whilst the control group went about their normal routine. It is therefore entirely possible that a reduction in depressive symptoms could be due to employees simply having some respite from their normal work stress to attend the intervention rather than the actual content. Although there were slightly greater effects for the CBT based studies compared to the others, there was still substantial variation in the content of the CBT interventions.
- Symptoms vs. illness. There’s no evidence that interventions can provide ‘true prevention’ of clinical depression. Although this review shows universal interventions may have small improvements for the mental health of a workforce, there’s no evidence that they prevent the onset of a clinically diagnosed depression. Therefore although the interventions might promote a slightly happier workforce, we don’t know if they would prevent clinical depression that results in people needing to stop work.
It’s worth noting that two of the authors work for an organisation that actually provides mental health training for workplaces (the Black Dog Institute in Australia). It is possible that this affiliation encouraged the authors to be overly optimistic about the benefits of workplace interventions.
In summary, Tan et al have shown that workplace interventions are associated with small reductions in depressive symptoms. However, their conclusions could be more cautious. More research is needed to understand what specific factors are most beneficial to employees’ symptom scores and whether interventions can prevent full-blown mental health disorders.
In the meantime, you might want to…
Links
Tan L et al. Preventing the development of depression at work: a systematic review and meta-analysis of universal interventions in the workplace. BMC Medicine 2014, 12:74 doi:10.1186/1741-7015-12-74
Harvey SB, Henderson M, Lelliott P, Hotopf M: Mental health and employment: much work still to be done. Br J Psychiatry 2009, 194:201–203. [Abstract]
Henderson M, Harvey SB, Overland S, Mykletun A, Hotopf M. Work and common psychiatric disorders. J R Soc Med 2011, 104:198–207.
Mathers CD, Loncar D: Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006, 3:e442.
World Health Organization/World Economic Forum. Preventing Non-communicable Diseases in the Workplace through Diet and Physical Activity. Report of a joint event (PDF). Geneva: World Health Organization; 2008.
Hamberg-van Reenen HH, Proper KI, van den Berg M. Worksite mental health interventions: a systematic review of economic evaluations. Occup Environ Med 2012, 69:837–845. [Abstract]
Tomlin, A. MoodGym no better than informational websites, according to new workplace RCT. The Mental Elf, 20 Sep 2012.
Tomlin, A. Making workplace adjustments for people with mental health problems: new guidance from the Department of Health. The Mental Elf, 13 Sep 2012.
Tomlin, A. Early intervention helps reduce depression and long-term sickness absence in office workers. The Mental Elf, 8 Sep 2011.
Tomlin, A. Women who work long hours are at risk of depression and anxiety. The Mental Elf, 13 Jul 2012.

RT @Mental_Elf: Preventing workplace depression: are there universal interventions that work? http://t.co/A1QQ8J23Em
@Mental_Elf what about the common sense “universal interventions” like good management, reasonable workload… Anything on that?
@inductivestep @Mental_Elf I think what’s really needed is a wider cultural shift towards valuing and looking after our wellbeing better :)
@Lauren_Bishop_ @Mental_Elf Indeed! :)
@Lauren_Bishop_ @Mental_Elf how often do people say: “I don’t know why she got depressed; lovely place to work, friendly folk & great boss”?
@Lauren_Bishop_ @Mental_Elf another universal intervention idea https://t.co/pP3EoOthnw
Preventing workplace depression: are there universal interventions that work?: Mental health in the workplace … http://t.co/flC4EeFo2A
@Mental_Elf One thing many organisations need is a robust and transparent policy on bullying and harassment.
Preventing workplace depression: are there universal interventions that work? Review cautions overly simplistic view http://t.co/K3XuZmqXFu
The Mental Elf liked this on Facebook.
Today @LaurenceDCP highlights a recent review of interventions to prevent depression at work http://t.co/A1QQ8J23Em
PRT @Mental_Elf: @LaurenceDCP highlights recent review of interventions to prevent #depression @ work http://t.co/LE0wDoIXyK @SupportMuted
Mental Elf: Preventing workplace depression: are there universal interventions that work? http://t.co/w8zT1El3Sx
Preventing workplace depression: are there universal interventions that work? – The Mental Elf http://t.co/aY9e990lXP
Do universal interventions to prevent workplace depression work? http://t.co/kGMBhzGw4o via @Mental_Elf
Hampshire Healthcare Library Service liked this on Facebook.
Mental disorders are the leading cause of sickness absence worldwide http://t.co/A1QQ8J23Em
RT @Mental_Elf: Depression is predicted to be the leading cause of work disability by 2020 http://t.co/A1QQ8J23Em
How well do workplace interventions for depression work? @LaurenceDCP explores latest research (via @Mental_Elf) http://t.co/OJ1VaZBszU
#Depression is predicted to be the leading cause of work #disability by 2020 http://t.co/W7JDDH6Uc9 << great review from @Mental_Elf
Los trastornos mentales son la principal causa de absentismo laboral por enfermedad. Prevenir puede funcionar: http://t.co/Aqgy8pMm5V
Preventing workplace #depression: are there universal interventions that work? http://t.co/RmXH75Kas0 http://t.co/yEFrveyJLs
“There’s good evidence that universal workplace mental health interventions can reduce depression”, says new SR http://t.co/A1QQ8J23Em
RT @Mental_Elf: Don’t miss: Preventing workplace depression: are there universal interventions that work? http://t.co/7DJve18YxH
Depression predicted to be leading cause of work disability by 2020. How can we prevent this from becoming a reality? http://t.co/YGaXWN1jmd
MRT @Mental_Elf: “good evidence universal workplace #mentalhealth interventions can reduce #depression” http://t.co/fXyLq7mz4W @supportmuted
Preventing workplace depression – http://t.co/LvisjGBPNt
“Preventing workplace depression: are there universal interventions that work?” http://t.co/Jf1St7CbHl
Nicola Davies liked this on Facebook.
How to prevent the #workplace #depression http://t.co/uBzAcpRQ7h
Preventing workplace #depression: are there universal interventions that work? asks @LaurenceDCP for @Mental_Elf http://t.co/6cNQi98trk
Preventing workplace depression: are there universal interventions that work? http://t.co/ubWSmHSwF1 via @sharethis
Interesting review of recent research on depression in the workplace – do interventions work? http://t.co/v2KzYkhe4R
Nicola Davies liked this on Facebook.
Hampshire Healthcare Library Service liked this on Facebook.
The Mental Elf liked this on Facebook.
[…] We need to know more about how to protect and improve mental health as a workplace asset. Prevention is a major focus of interest in workplace mental health going forward, but the evidence for interventions are in their infancy, a topic covered by Laurence Palfreyman in a Mental Elf blog in June 2014. […]