
There is evidence to suggest that people with diabetes are twice as likely to suffer from depression. It’s therefore important that the cost-effectiveness of treatments for comorbid depression be indentified.
The elves have already reported on a review of the effectiveness of collaborative care for people with diabetes and depression, suggesting that the intervention might be effective. While there are many cost-effective treatment options for depression, it does not necessarily follow that these treatments will be effective and cost-effective for people with diabetes.
It’s possible that people with diabetes do not have the same capacity to benefit from treatment for depression, because of the impact of their diabetes on quality of life. Alternatively, it’s possible that individuals receiving treatment for diabetes might not be able to also engage fully with treatment for depression – or vice versa.
Furthermore, comorbid diabetes and depression is likely to affect the way people use health services, with important implications for the costs of care.
A new systematic review by Jeeva and colleagues summarises the existing evidence for the cost-effectiveness of treatment for depression in people with diabetes.
Methods
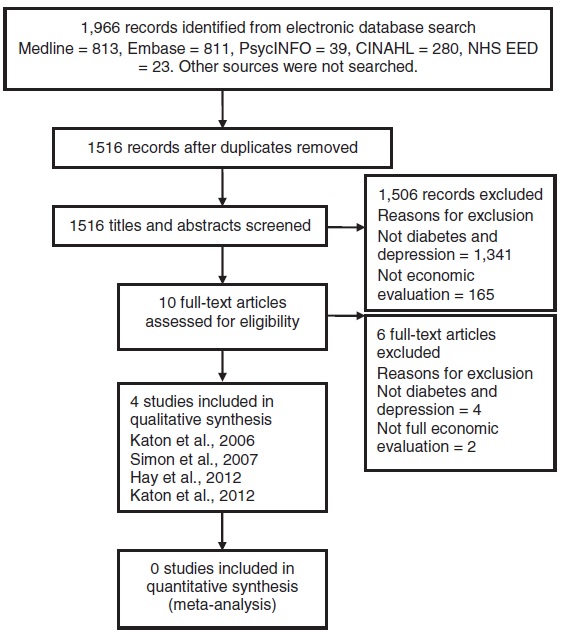
The authors searched Medline, Embase, PsycINFO, CINAHL, and NHS EED databases. Only full economic evaluations of interventions to manage depression in people with diabetes, published between January 2000 and May 2012, were included.
Results
The review identified only 4 economic evaluations of treatment for depression in people with diabetes.
The samples included in the studies varied, with some studies targeting specific age groups or ethnicities. All interventions evaluated in the 4 studies included some form of collaborative care with stepped care plans or care management alongside psychotherapy and/or antidepressants. The choice of outcome measure differed across studies, including depression free days and quality adjusted life years (QALYs). All four studies reported a net benefit associated with the intervention being evaluated. Three of the 4 studies reported net cost savings, but none of these differences were statistically significant.
Discussion
My own back-of-the-envelope estimates suggest that as many as 750,000 people with diabetes suffer from comorbid depression in the UK alone. Considering that such a large population is affected, the following limitations of the existing body of research are surprising:
- All studies were carried out in the USA
- One author was involved in all the studies
- None of the studies were adequately reported
- Usual care was not described in any of the papers
- It is unclear whether any of the studies had sufficient sample sizes to detect differences in cost-effectiveness
- None of the studies reported direct non-medical costs
- None of the studies carried out sensitivity analyses to assess generalisability to other settings or countries
- None of the studies reported full resource use and unit cost data, preventing transferability of estimates
- None of the studies reported on adherence, despite identifying this as potentially important
- None of the studies accounted for clustering effects
- Three of the 4 studies did not identify whether participants had Type 1 or Type 2 diabetes
- Only 1 study addressed the problem of missing data
The authors of the review also identify a number of limitations in their own study, admitting that they may have missed important studies from grey literature. These issues mean that the validity of the cost-effectiveness estimates is limited, particularly for readers outside the USA. There is a need for more research in other settings, with extrapolation to the long-term.
-
These studies’ cost-effectiveness results are not generalisable outside the USA, where prices are higher than in most other countries
Conclusion
The authors conclude that:
Economic evidence suggests that from a U.S. payers perspective, collaborative care to manage depression in people with diabetes is associated with gains in health benefit and may be cost saving.
However, this statement is subject to many caveats, as outlined above. Clearly this is an area where more research is needed. The large number of people affected by comorbid diabetes and depression, and the possibility that the interventions identified in this review are both health-improving and cost-saving, suggests that further research could be highly cost-effective. It’s vital that future economic evaluations are reported in a consistently comprehensive and systematic fashion, following the Consolidated Health Economic Evaluation Reporting Standards (CHEERS).

This review highlights the importance of following good practice guidelines for the reporting of research
Links
Jeeva, F., Dickens, C., Coventry, P., Bundy, C., & Davies, L. Is treatment of depression cost-effective in people with diabetes? A systematic review of the economic evidence. International Journal of Technology Assessment in Health Care 2013, 29(4), 384–91. [PubMed]
Huang, Y., Wei, X., Wu, T., Chen, R., & Guo, A. Collaborative care for patients with depression and diabetes mellitus: a systematic review and meta-analysis. BMC Psychiatry 2013, 13(1), 260. [PubMed]
Husereau, D., Drummond, M., Petrou, S., Carswell, C., Moher, D., Greenberg, D. et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMC Medicine 2013, 11(1), 80. [PubMed]

Is treatment for depression cost-effective in people with diabetes?: There is evidence to suggest that people … http://t.co/PqLGuPO94B
Mental Elf: Is treatment for depression cost-effective in people with diabetes? http://t.co/CcbHP6PyHJ
Our resident economics expert @ChrisSampson87 blogs about the cost-effectiveness of treating depression in diabetes http://t.co/SNjLfj5phC
New post by me on @Mental_Elf covering economic evidence for treatment of comorbid depression in people with diabetes http://t.co/8MbCvfGCBH
Evidence suggests that people with diabetes are twice as likely to suffer from depression http://t.co/SNjLfj5phC
Is treatment for depression cost-effective in people with diabetes? – The Mental Elf http://t.co/e9vpY6qaih
Is #treatment for depression cost-effective in people with #diabetes? http://t.co/JSicB7o81G http://t.co/Vf0DcZW26p
@ChrisSampson87 blogs on the cost-effectiveness of treatment for comorbid depression in people with diabetes http://t.co/SNjLfj5phC
In case you missed it: Is treatment for depression cost-effective in people with diabetes? http://t.co/SNjLfj5phC
.@Mental_Elf Is the depression caused B Vit deficiency assoc with scripted Metformin/anti-epileptics prescribed for neuropathy? Worth study?
RT @Mental_Elf: In case you missed it: Is treatment for #depression cost-effective in people with #diabetes? http://t.co/cIjObuqAvw
“@Mental_Elf: In case you missed it: Is treatment for depression cost-effective in people with diabetes? http://t.co/ZObXz3I3Pk” interesting
RT .Mental_Elf: Never Forget: Is treatment for depression cost-effective in people with diabetes? http://t.co/ABXbItxDAg
@Mental_Elf review on providing treatment for depression in diabetes care #mentalhealt http://t.co/m3StcyEM5n
cognitive analytic therapy is a proven cost effective treatment for those with diabetes who have psychological issues including depression, diabulimia, anxiety and so on, and whose poor control is implicated within this.