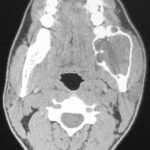
Ameloblastoma is an uncommon benign but locally aggressive odontogenic tumour. Earlier this week (Dental Elf – 13th Feb 2019) we looked at a review that estimate a pooled global incidence rate of 0.92 per 1,000,000 person‐years (95%CI;0.57–1.49). Surgery is the main treatment choice, typically separated into conservative or radical methods dependant on tumour type and clinical presentation. Unicystic and peripheral ameloblastoma are usually treated conservatively, while solid or multicystic ameloblastoma are often treated radically.
The aim of this review was to assess the outcomes of radical and conservative treatment approaches for solid or multicystic as well as unicystic ameloblastoma in terms of recurrence rates.
Methods
Searches were conducted in the PubMed, Embase, Scopus and Web of Science databases. English language studies published between 1969 and 2018 presenting information on ameloblastoma treatment and recurrence rates with histological diagnosis of tumour type were considered. Care reports and studies providing fewer than 10 cases were excluded.
Two independent reviewers selected studies and abstracted data. Risk of bias was assessed using the Quality Appraisal of Case Series Studies Checklist (QACSS) by Institute of Health Economics (IHE). The main outcome was recurrence rates. These were calculated for treatment approach and tumour type.
Results
- 20 studies reporting 1069 cases of ameloblastoma (218 recurrences) were included.
- All 20 studies were retrospective.
- Data was included from 15 countries with follow up times ranging from 1month – 25 years.
- Only 5 studies met >70% of the quality criteria.
- Solid or multicystic ameloblastoma
- For radical treatment the pooled recurrence rate (15 studies, 364 ameloblastoma) = 8% (95% CI, 4–13%).
- For conservative treatment the pooled recurrence rate (11 studies, 341 ameloblastoma) = 41% (95% CI, 34–48%).
- Unicystic ameloblastomas
- For radical treatment the pooled recurrence rate (12 studies, 109 ameloblastoma= 3% (95% CI; 1–7%).
- For conservative treatment the pooled recurrence rate (15 studies, 255 ameloblastoma) = 21% (95% CI, 16–26%).
Conclusions
The authors concluded: –
The present systematic review and meta‐analysis showed statistically significant results favouring radical treatment for both unicystic and solid or multicystic ameloblastoma. The solid or multicystic ameloblastoma may behave more aggressively than the unicystic ameloblastoma based on the recurrence rates. The evidence of the results is limited since only retrospective studies were available.
Comments
This review found that pooled recurrence rates for solid ameloblastomas were 8% after radical, and 41% after conservative treatment with values for unicystic ameloblastomas being 3% and 21%, respectively. While the reviews findings favour a radical approach for both types of ameloblastoma there are a number of important considerations. All the included studies were retrospective case series which a more likely to have selection and reporting biases and as the authors noted that was a lack of important information regarding descriptions of the surgical approach, length of follow up. There was also a lack of data on complications, adverse effects or quality of life data, or other psychological, functional or aesthetic impacts of treatment. Further high quality well-reported prospective studies that include long-term clinical and patient focuses outcomes are needed.
Links
Primary Paper
Hendra FN, Natsir Kalla DS, Van Cann EM, de Vet HCW, Helder MN, Forouzanfar T. Radical vs conservative treatment of intraosseous ameloblastoma: Systematic review and meta-analysis. Oral Dis. 2018 Dec 12. doi: 10.1111/odi.13014. [Epub ahead of print] Review. PubMed PMID: 30548549.
Other references
Dental Elf – 13th Feb 2018
Picture Credits
By Berto1286 – Own work, Public Domain
