
[Note: this blog was published on 6/5/15 and amended on 7/5/15. As a shining example of crowd sourced peer review in action, a duplication was spotted by an attentive reader, which affects the results of the meta-analysis. The authors of the meta-analysis were contacted, they promptly responded, and updated results were given. The update is explained in more detail in the results section below.]
I should declare a couple things here.
Firstly, I’m involved in a research group whose focus is on developing psychological treatments for Post-Traumatic Stress Disorder (PTSD), broadly categorised as Trauma-Focused Cognitive Behavioural Therapy (TF-CBT).
Secondly, I’m a psychologist. Which in some respects means that my preference and knowledge both centre around psychological treatments over pharmacological. However, despite a lot of recent tribalism (See Mental Elf’s brilliant reflections on the issue here) I firmly believe healthcare benefits from plurality, and people should have a choice of treatments that work for them, be they psychological or not.
Having said that, psychological treatments, namely TF-CBT or Eye Movement Desensitisation and Reprocessing (EMDR), are favoured, at least in England, as first line treatment recommendations for PTSD, whereas pharmacotherapy is recommended as a second-line intervention in certain circumstances, for example, where the person expresses a preference against TF-CBT, or where there is serious threat of ongoing trauma, or in the treatment of sleep difficulties (see NICE, 2005). In Australia, similar conclusions were recently drawn in updated guidelines (ACPMH, 2013).
However, in light of updated evidence and new DSM-V criteria for PTSD, the NICE guidelines are currently being reviewed. So at least in England, these recommendations may soon change.
With all this in mind, I was intrigued to review a recent systematic review and meta-analysis published in the British Journal of Psychiatry, exploring the efficacy of pharmacotherapy for the treatment of PTSD (Hoskins et al, 2015). Essentially, this paper serves as an update on the evidence since the 2005 NICE guidelines were produced.

In the UK, drug therapy is very much a second-line intervention (behind talking treatments) for people with PTSD.
Methods
All double-blind, randomised, placebo-controlled comparative trials of the efficacy of pharmacological interventions for PTSD were included. Many of these were also included in the original NICE guidelines and Cochrane review conducted at the time (Stein et al., 2006).
Outcome measures were both clinician-rated (using the Clinician Administered PTSD Scale; CAPS; as gold standard) and self-report (using the Davidson Trauma Scale; DTS; as gold standard).
A large number of databases were searched; including Medline, EMBASE, HMIC, PsycINFO, ASSIA, CINAHL, WHO regional databases, PILOTS, the Cochrane Library, the Controlled Trials Register, Web of Knowledge, OpenSIGLE and Google Scholar.
Trials were excluded if TF-CBT was initiated or ongoing. Open label trials were also excluded.
PRISMA guidelines were followed.
Results
Study characteristics
Once duplicates were removed, 9,095 studies were identified in total. Once irrelevant and excluded studies were removed, a total of 51 studies were included in the review.
The average sample size was 130, mean age was 41 and 54% of participants were women. The majority of included studies were conducted in the USA. None of the included studies were conducted solely in the UK.
Studies focused on a range of traumatic incidents. Primarily these were combat and physical/sexual assault. A smaller number of studies focused on natural disaster and road traffic accidents.
The majority of trials studied SSRIs (31), with the others investigating tricyclics, monoamine oxidase inhibitors, and other antidepressants.
Efficacy of pharmacotherapy
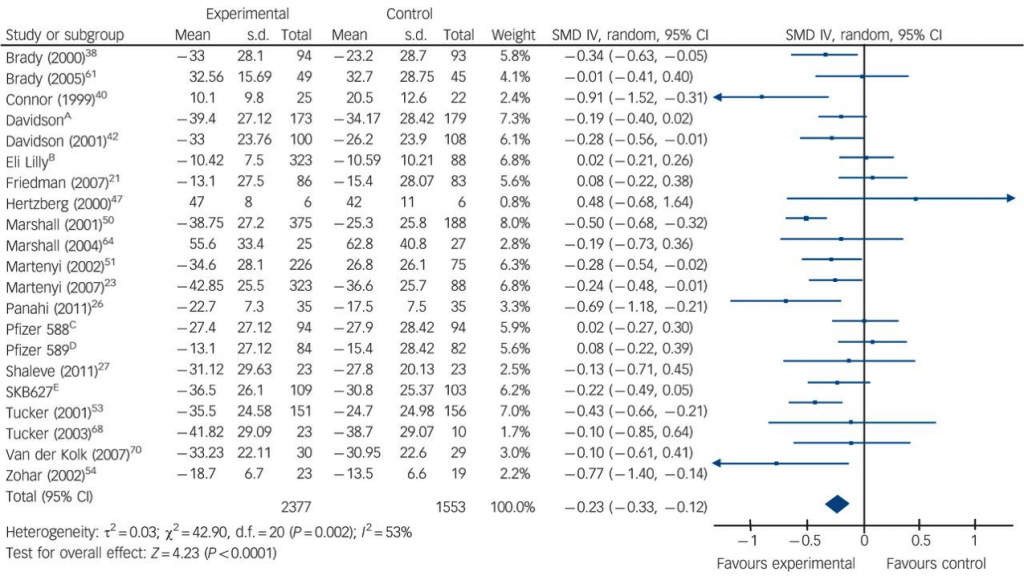
A meta-analysis of SSRI versus placebo was undertaken using 21 studies. The results favoured SSRIs, though the effect size was small (ES 0.23, 95% CI, 0.12 to 0.33).
In terms of individual drugs, paroxetine was significantly superior to placebo on both CAPS and DTS scores. Fluoxetine and venlafaxine were significantly superior to placebo on CAPS scores alone.
Amendment (added 7/5/15)
Associate Professor at the Oxford University Department of Psychiatry, Andrea Cipriani, got in touch with the Mental Elf via email, alerting us to the possibility that two pairs of studies included in the meta-analysis appeared to have highly similar characteristics on the funnel plot (see figure 1). He also posted the following on the blog page:
Dear Mental Elf,
Looking at the original paper by Hoskins et al., 2015… it seems to me that the authors counted twice in the forest plot two studies (namely, Eli Lilly as the same study as Martenyi 2007 and Pfizer 589 as the same as Friedman 2007).
It would be nice if the authors (and the journal) could clarify this issue.
Indeed, although not identical, both pairs of studies showed highly similar characteristics.
We pursued the issue by posting comments on the blog and approaching the authors of the review via twitter. Mat Hoskins (co-author) responded very quickly, via a blog comment, with the following:
Hi Prof Cipriani, many thanks for your comment, you were quite right and we did send a reply back to BJP. The meta-analysis now shifts in statistically significant favour for sertraline, in addition to paroxetine, venlafaxine and fluoxetine.
So essentially, the duplicated trials changed the outcome of the meta-analysis, most notably by removing one of the included studies reporting that sertraline performed worse than placebo. In doing so, sertraline became significantly favoured to placebo overall.
The interesting power of placebo
This could almost be a heading of its own in pharmacotherapy trials. Its fascinating. In this case, placebo accounted for over 40% symptom reduction in some trials, however this varied.

The evidence was strongest for fluoxetine, paroxetine and venlafaxine, as these were the only drugs that were statistically superior to placebo.
Conclusions
In simple terms, the authors conclude that:
This systematic review found statistically significant evidence on meta-analysis for three pharmacological agents v. placebo in the treatment of PTSD (fluoxetine, paroxetine and venlafaxine) but no evidence for brofaromine, olanzapine, sertraline or topiramate.
[Although since the amendment, sertraline is now favoured v. placebo as well].
However, they also observe that the effect is small in comparison to certain psychological treatments:
The effect sizes for pharmacological treatments for PTSD compared with placebo are low and inferior to those reported for psychological treatments with a trauma focus over waiting-list or treatment as usual controls.
However, the authors raise a useful point. Because the included trials focused on monotherapy interventions, they were unable to conclude as to whether pharmacotherapy can augment psychological interventions for PTSD. This would be valuable information, given many people receive both.

Combined psychotherapy and antidepressant treatment works well for many mental health conditions, but this review does not tell us if this combination may also work for PTSD.
Limitations
Heterogeneity
There was considerable clinical and statistical heterogeneity between studies included in the meta-analysis.
Risk of bias
Despite all 51 studies describing themselves as double-blind, only eight studies adequately report on the process in order to adequately determine low risk of bias (according to the authors).
Also as the authors point out, because only a number of studies (41 of the 51) included intention to treat (ITT) analyses, there is a risk of publication bias in terms of outcome reporting, particularly if participants withdrew from trials due to adverse effects, greater severity of symptoms or a perceived lack of efficacy.
Summary
This review provides a useful update on the evidence included in national guidelines for supporting people with PTSD in the UK. Certain SSRIs appear effective, though effect sizes are smaller than recommended psychological treatments. Only paroxetine was significantly superior to placebo on both clinician and patient-rated measures.
We aren’t able to ascertain the efficacy of combining these treatments and study limitations were evident.
Also, it raises an interesting question about what precisely is being treated in PTSD, which isn’t answered by the review. Certainly psychological interventions will at least in part be designed to confront and update the trauma memory and, in the case of TF-CBT, develop strategies to manage the difficult thoughts and associated feelings (see Ehlers et al., 2005). SSRIs, it seems, are aimed at a symptom level. Again, provided there is evidence for the efficacy of both, patient choice seems important here.
It will be interesting to see what changes, if any, are made when the NICE guidelines for PTSD are updated.

It’s been a decade since the NICE PTSD guideline was published, so it’ll be interesting to see if this new evidence encourages an update.
Reflections on the amendment
- Firstly, the process clearly showed me how easily important factors can be missed. Indeed, the duplication had made it through peer review before being published, as well as subsequent comment by the journal. I missed it too.
- Secondly, the process demonstrated, for me at least, the importance of crowd-sourced peer review. It was through an active online discussion, involving bloggers, readers and authors, that the error was highlighted and amended. The whole process took less than 24 hours.
- Lastly, it reiterated the fundamental importance of transparency. Discussion that is frank, open and publicly visible means that oversights can be identified and put right.
Links
Primary paper
Hoskins M, Pearce J, Bethell A, Dankova L, Barbui C, Tol WA, van Ommeren M, de Jong J, Seedat S, Chen H, Bisson JI. Pharmacotherapy for post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry. 2015 Feb;206(2):93-100. doi: 10.1192/bjp.bp.114.148551.
Other references
ACPMH (2013). Australian Guidelines for the Treatment of Acute Stress Disorder and Posttraumatic Stress Disorder. Australian Centre for Posttraumatic Mental Health, 2013.
Ehlers A, Clark DM, Hackmann A, McManus F, Fennell M. (2005) Cognitive therapy for post-traumatic stress disorder: development and evaluation. Behaviour Research and Therapy, 43, 413-431. [PubMed abstract]
NICE (2005). Post-traumatic stress disorder (PTSD): The management of PTSD in adults and children in primary and secondary care [CG26]. London: NICE.
Stein DJ, Ipser JC, Seedat S. Pharmacotherapy for post traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews 2006, Issue 1. Art. No.: CD002795. DOI: 10.1002/14651858.CD002795.pub2.

@Mental_Elf see @ptsdresolution website evidence based #therapy it works, enough said!
Pharmacotherapy for PTSD: an update on the evidence finds some efficacy but… http://t.co/BShfmOgcGQ #MentalHealth http://t.co/wltl2lsnXo
Pharmacotherapy for PTSD: an update on the evidence finds some efficacy but small effect sizes: Patrick Kenned… http://t.co/Fyw6lhu9B2
Pharmacotherapy for PTSD: an update on the evidence finds some efficacy but small effect sizes https://t.co/TDmcu7WQ1m via @sharethis
Today @paddy_kw on a recent systematic review of pharmacotherapy for #PTSD http://t.co/YBI19n0O7X
Do SSRIs work for PTSD? http://t.co/m7RU4vKyw1
Hoskins M et – pharmacology of #ptsd: still no evidence on combined treatment http://t.co/244G7enylO via @Mental_Elf http://t.co/6PLPmLbOF3
Pharmacotherapy for #PTSD: an update on the #evidence finds some efficacy but small effect sizes http://t.co/zLmA9cKlAQ from @Mental_Elf
Dear Mental Elf,
looking at the original paper by Hoskins et al., 2015 (Figure 2 of the published article and online data supplement) it seems to me that the authors counted twice in the forest plot two studies (namely, Eli Lilly as the same study as Martenyi 2007 and Pfizer 589 as the same as Friedman 2007).
It would be nice if the authors (and the journal) could clarify this issue
Best wishes
Andrea Cipriani
(University of Oxford – @And_Cipriani)
Pharmacotherapy for PTSD: an update on the evidence finds some efficacy but small effect sizes http://t.co/6OTBxjNYjr
http://t.co/m7RU4vKyw1 SSRIs for PTSD. @And_Cipriani raises a potential duplication issue with the meta analysis. Any ideas from @rcpsych?
Recent SR finds little evidence to recommend #antidepressants over psychotherapies for #PTSD http://t.co/YBI19n0O7X
Hi @dochosk We’ve blogged about your pharmacotherapy for #PTSD review http://t.co/YBI19n0O7X Pls let us know what you think @paddy_kw
Specifically @dochosk Did you double count studies in yr SR as suggested by @And_Cipriani in our comments? http://t.co/YBI19n0O7X @paddy_kw
@Mental_Elf @And_Cipriani @Paddy_kw hi great article, Prof Cipriani was right and a correction was sent back to BJP cont’d.
@Mental_Elf @And_Cipriani @Paddy_kw revision recommends paroxetine, venlafaxine, fluoxetine and now sertraline as 2nd line.
@dochosk @Mental_Elf @And_Cipriani @Paddy_kw I’ve always heard Sert was s2nd line but I was put on it immediately at a high dose – confused
@dochosk @Mental_Elf @And_Cipriani @Paddy_kw That should be 2nd, I cannot do the typing thing today
@dochosk @Mental_Elf @And_Cipriani Mat – so to confirm.. both pairs were duplicates? Friedman & Pfizer is more obvious.
@Paddy_kw @Mental_Elf @And_Cipriani that’s right and Eli Lily was Martenyi 2007.
@dochosk @Mental_Elf @And_Cipriani great thanks. I’m amending the blog.
Don’t miss: Pharmacotherapy for #PTSD http://t.co/YBI19n0O7X #EBP
“@Mental_Elf: Don’t miss: Pharmacotherapy for #PTSD http://t.co/Io35lAPs30 #EBP” @jack8656 FYI
@Mental_Elf excellent blog summarizing a recent systematic review and meta-analysis of pharmacotherapy for #PTSD
Pharmacotherapy for #PTSD: an update on the evidence finds some efficacy but… http://t.co/BShfmOxNyo #MentalHealth #vets
Mental Elf: Pharmacotherapy for PTSD: an update on the evidence finds some efficacy but small effect sizes http://t.co/Hu9C3TraVC
Pharmacotherapy for PTSD: an update on the evidence finds some efficacy but small effect sizes https://t.co/gDdY1Vfl0c via @sharethis
Thanks again to @dochosk & @And_Cipriani for comments on @Paddy_kw’s #PTSD blog yesterday. Updated version here: http://t.co/YBI19n0O7X
@Mental_Elf @And_Cipriani @Paddy_kw and thanks for the great blog. Hopefully the amendment will be in BJP soon!
Pharmacotherapy for PTSD: an update on the evidence finds some efficacy but small effect sizes https://t.co/NQA4ilLD0w via @sharethis
Pharmacotherapy for PTSD http://t.co/T4MVlkzFZ3
#Pharmacotherapy for #PTSD: an update on the evidence finds some efficacy but small effect sizes http://t.co/46iZ9dtnSu