
“The future is digital”
So it has been said many times. In April 2017, NHS England assigned (up to) £70m to seven trusts to develop digital mental health technology in a bid to curb some of the pressure that mental health services are under (Merrett, 2017).
When we hear about eHealth it is often accompanied by buzz words like ‘innovation’, ‘revolution’ and ‘frontier’ which get people excited and hopeful, but it is soon followed by disillusionment. The problem with web-based interventions for mental health disorders is that even when the intervention is shown to have efficacy, the research findings don’t translate into clinical settings and there is a lack of buy-in from staff and service users. Hence, digital technology for mental health is like that Nutribullet you bought, used twice and now sits on your shelf collecting dust because it’s too much effort to use frequently and you never have all the ingredients.
Fortunately, research is starting to look beyond the development and effectiveness of online interventions and is now considering how these can be scaled up and successfully implemented in real world settings. This year Lobban and colleagues published a paper in the Journal of Medical Internet Research on the feasibility and acceptability of web-based Enhance Replapse Prevention for Bipolar Disorder (ERPonline) (Lobban et al., 2017). This online intervention was designed purposely for managing early warning signs (EWS) of relapse and developing effective coping strategies for bipolar.
A new paper from this group (Dodd et al., 2017) has just been published in the Evidence Based Mental Health journal. Usefully, this focuses on the users’ experience of ERPonline.

Is investment in digital mental health interventions really just like wasting money on a fancy juicer?
Methods
ERPonline is a self-directed web-based intervention to be used by people with bipolar. The modules choices can be seen in Figures 1 and 2 below (Lobban et al., 2017).
Setting the scene (what you need to know):
The original feasibility study of ERPonline (Lobban et al., 2017) involved 96 participants being randomly allocated to receiving either ERPonline for 12 months or to a waitlist control. Participants were contacted by researchers via telephone every 12 weeks to complete interview-rater outcome measures. Additionally, participants were contacted by an unblinded member of the research team two weeks before the follow-up assessments to encourage retention and provide people with the opportunity to ask questions or raise concerns about the study.

Figure 1. ERPonline home page (Lobban et al., 2017). View larger version of this image.
Qualitative interviews
The group that received ERPonline (n=46) were invited to take part in qualitative interviews asking about:
- Participation in research
- Barriers and facilitators to using ERPonline
- Reflections on using online support
A framework approach was used to support thematic analysis because specific ideas were being explored and this method provides a more structured way of managing and mapping the data.
Transcripts were initially rated by two independent researchers to get a coding frame with themed headings. Once these were tested on a small number of transcripts, they were checked by the Service User Reference Group for feedback on the interpretation of the transcript before it was applied to all.
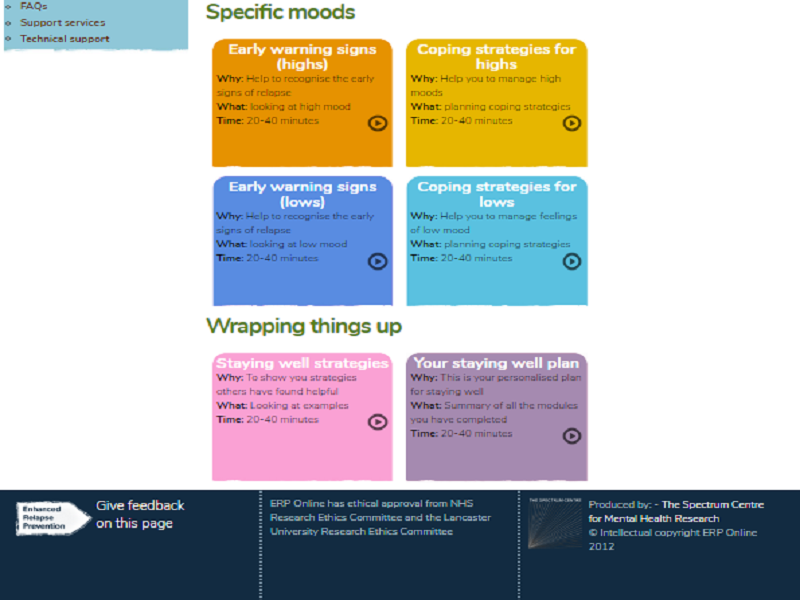
Figure 2: ERPonline home page continued. View larger version of this image.
Results
19 people were interviewed. Most participants had bipolar I (only two people had bipolar II) and were high functioning (low relapse, more education and employed).
The average number of visits to the ERPonline site was 85.
Key findings about taking part in the study
- People like human contact! High retention rates were largely due to interaction with the researchers
- Other factors that motivated people to stage engaged were: the perceived trustworthiness of research team as sources of information and expertise, participation in the study was flexible and could work around their schedule, the potential for ERPonline to be helpful
Key facilitators and barriers to using ERPonline
- People like the interactive and personalised elements. The most frequently visited modules were life and mood charting modules
- Time constraints and privacy were the main issues with the intervention. People wanted to use it alone and didn’t want it seen in public, at work or in front of family/friends
- Mood was a barrier for some (when unwell), but a facilitator for others (offered support when experiencing symptoms)
Reflections on using online support
- ERPonline may also be useful for relatives/carers of people with bipolar
- The intervention was thought of as maintaining/reinforcing usual care
- Easily integrated and can be shared with their clinician or care coordinator but should not be seen as a replacement for face-to-face support
Conclusion
- Online interventions should supplement human contact in the management of bipolar disorder
- Personalisation is important so individual preferences can be taken into account.

This study concluded that digital interventions should work alongside face-to-face support, rather than be seen as a replacement for them.
Limitations
The authors accurately identify that their main limitation is their sample. They did not recruit anyone from the WLC group for the interviews and those in the intervention group that were interviewed were high functioning with low relapse rates. It’s not a representative group and may have affected participants’ engagement with ERPonline. That aside, it’s a good quality feasibility study (++ using the ‘Quality Assessment for Qualitative Studies checklist’ from NICE) and it does what it says on the tin.
Implications
Clinical implications include “appropriate resourcing for web-based interventions, particularly around technical and non-technical support” (Dodd et al., 2017). This is an important point that needs emphasising. One of the challenges faced by online interventions is the ability to integrate them within NHS computer systems, which have been described by many as “archaic”. NHS systems are unlikely to change at any great speed so this needs to be taken into account early on when digital mental health technology is being developed. A recent paper by Mohr et al., 2017 suggests that we need to stop seeing mental health technologies as a product (and the main cause of change) and start seeing these interventions as “services that are supported by technologies”. In this study, ERPonline could be a service that provides monitoring of mood, recognition of triggers and early warning signs of relapse in bipolar in conjunction with support by a care coordinator, rather than a stand-alone tool trying to change a person’s behaviour. Reconceptualising digital technology would result in all elements (the goal of services, the role of digital mental health interventions and the needs of service users) being considered at the same time when online interventions are being designed and evaluated (Mohr et al., 2017).
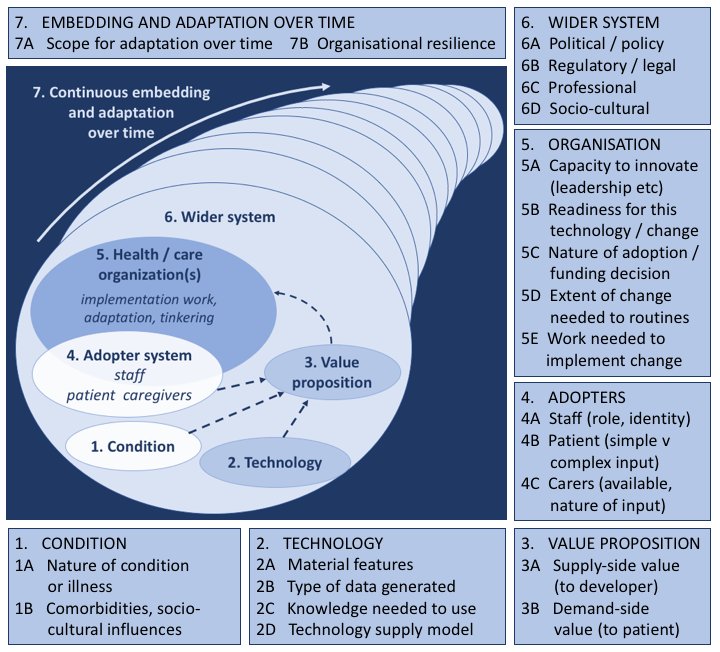
Just a few weeks ago, a new framework called NASSS (nonadoption, abandonment, scale-up, spread, and sustainability, Figure 3) was published for predicting and evaluating the success of technology-supported health and social care programmes (Greenhalgh et al, 2017).
The seven domains in the NASSS framework can be categorised as ‘simple’, ‘complicated’ and ‘complex’ depending on the challenges faced in each component. Those that are considered ‘complex’ in several of the domains are rarely implemented successfully. This framework isn’t a checklist and still needs further testing, but it does provide some guidance for identifying and understanding the challenges that occur in integrating digital technology into health care programs.
Take home message
In March this year I went to a Digital Mental Health Question Time event. At that session one of the speakers said something that has stuck with me:
Stop talking about digital as magic. Talk about it as a tool…as part of a kit.
The message from people interviewed in this study of ERPonline reminds me of that. Perspectives on participating in the study and the online intervention were favourable, but ultimately what people want is a connection with other people. Part of our challenge going forward is to find the right mix of digital technology and human contact at the right time, and to manage our expectations.

What’s the right mix of digital technology and human contact for people experiencing different mental health difficulties?
Conflicts of interest
I was a peer reviewer for this paper (Dodd et al, 2017) published in the Evidence-Based Mental Health journal.
Links
Primary paper
Dodd AL, Mallinson S, Griffiths M, et al. (2017) Users’ experiences of an online intervention for bipolar disorder: important lessons for design and evaluation. Evidence-Based Mental Health 2017;20:133-139. ebmh.bmj.com/content/20/4/133
Other references
Lobban F, Dodd AL, Sawczuk AP, Asar O, Dagnan D, Diggle PJ, Griffiths M, Honary M, Knowles D, Long R, Morriss R, Parker R, Jones S. (2017) Assessing Feasibility and Acceptability of Web-Based Enhanced Relapse Prevention for Bipolar Disorder (ERPonline): A Randomized Controlled Trial. J Med Internet Res 2017;19(3):e85 DOI: 10.2196/jmir.7008
Greenhalgh T, Wherton J, Papoutsi C, Lynch J, Hughes G, A’Court C, Hinder S, Fahy N, Procter R, Shaw S. (2017) Beyond Adoption: A New Framework for Theorizing and Evaluating Nonadoption, Abandonment, and Challenges to the Scale-Up, Spread, and Sustainability of Health and Care Technologies. J Med Internet Res 2017;19(11):e367 DOI: 10.2196/jmir.8775

I remain sceptical, as I always have been, of online self help/monitoring. This sample size is very small, only including high functioning people with bipolar who are more likely to have the motivation to use this. Also the high level of support from researchers can be a strong factor in the drive to participate. In reality, such support from mental health is likely to be considerably lower. In theory it’s a good idea and I don’t wish to dismiss it entirely but I am aware that in reality paper based mood charts and tools such as WRAP is hard for many people to complete consistently. Bipolar 1 and 2 generally isn’t high functioning with motivation to complete or ability when depressed is extremely hard. On the hypomania/mania phases the charting would most likely not be on the radar. Commonly as we know, the more episodes experienced tends to create smaller gaps between episodes and/or symptoms in between. Over all my knowledge from a lot of experience with bipolar leads me to conclude that allocated mental health professionals – e.g. CPN’s are best placed to be physically present for meaningful collaborative working