
Excessive, debilitating, and persistent worry is a cornerstone of Generalised Anxiety Disorder (GAD), impairing one’s physical and mental health and daily functioning. GAD is a common disorder, affecting approximately 4-7% of people in the UK (Hoge, Ivkovic, & Fricchione, 2012). Drug treatments are often the first port of call, with previous research showing greater efficacy over psychological interventions (Bandelow et al, 2015). In spite of this, most GAD sufferers do not recover, and at least 1 in 4 do not respond to the most effective medications (Baldwin, Waldman, & Allgulander, 2011).
Research on the efficacy of newer drugs has stagnated, with limited incentive and funding. In light of this, the authors of this study chose to employ a strategy known as network meta-analysis (NMA) by which medications can be compared within and between trials against each other and placebos, yielding hierarchal evidence of pharmacological treatment efficacy (Faltinsen et al., 2018).

Many drugs are licensed for use in Generalised Anxiety Disorder (GAD), but it is unclear what works best.
Methods
The researchers conducted a systematic review of the available drugs for treatment of generalised anxiety disorder (GAD). Randomised controlled trials published between 1994 to 1997 were identified through online databases, clinical and commercial pharmaceutical registries, and grey literature.
The criteria for inclusion were:
- GAD diagnosis
- Comparison of a drug against another or placebo
- Adult outpatients
- Minimum of 10 participants per group
- Studies reporting change from initial measurement of anxiety
Studies were excluded if:
- Participants had multiple diagnoses (except depression)
- They used relapse prevention or discontinuation designs
The researchers sought to assess the efficacy and acceptability of the various drugs used for treatment of GAD.
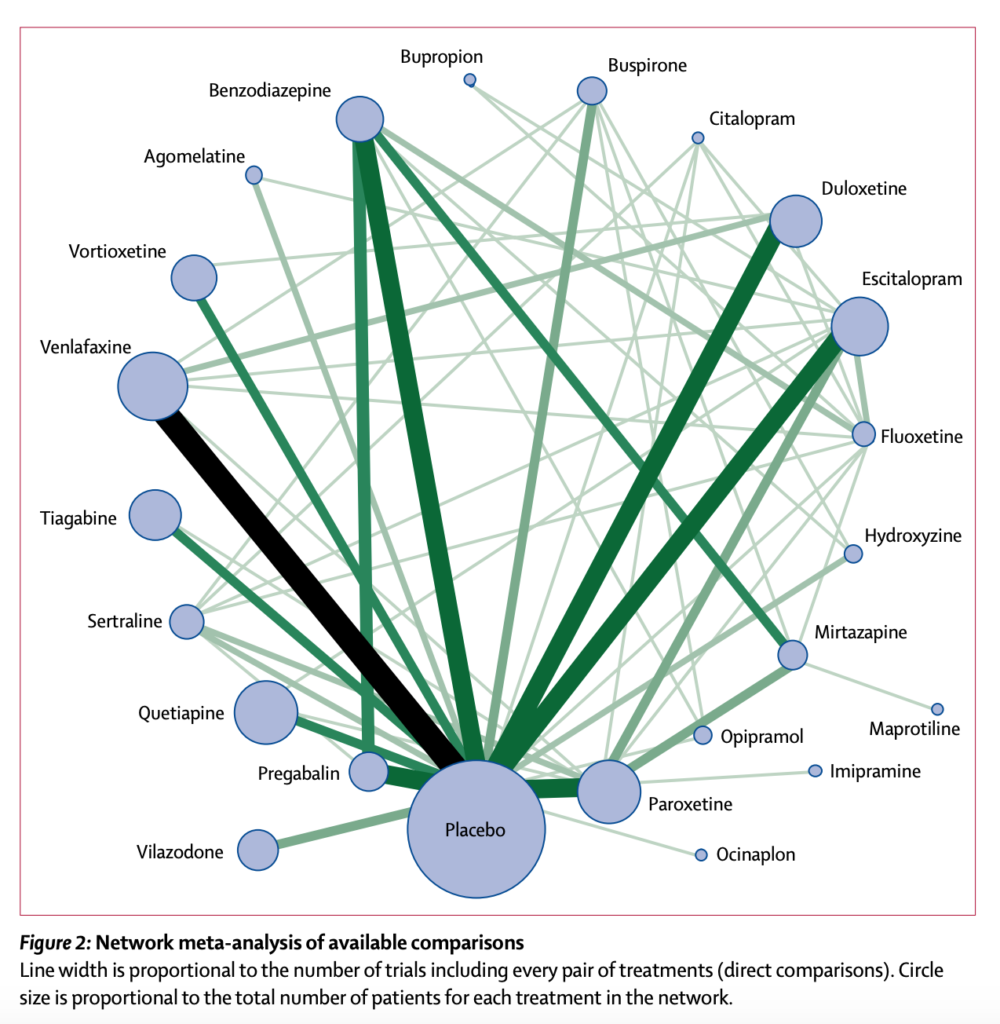
Figure 2: Network meta-analysis of available comparisons (reproduced from the original paper by Slee et al, 2019)
Results
89 studies met the inclusion criteria, with a total of 25,441 participants and 22 drugs. 63 trials compared the drug of interest against placebo while 45 included multiple active drugs.
Quetiapine yielded the largest reduction in anxiety symptoms, dropping by 3.6 points on the Hamilton Anxiety Rating Scale (HAM-A). However, patients taking this drug were less likely to complete the trial than those on placebo, indicating that it might not be well-tolerated. Similarly, paroxetine and benzodiazepines were found to reduce anxiety symptoms, but these were poorly tolerated and have limited use in practice due to addictive properties and side-effects.
Selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs) are recommended as cost-effective first-line drugs in NICE guidance despite having an incomplete evidence base. Although sample sizes were limited, this study showed that mirtazapine, sertraline, fluoxetine, buspirone, and agomelatine are well-tolerated and effectively reduce symptoms, consolidating current treatment guidelines. Meanwhile, pregabalin, indicated for patients who do not tolerate such drugs, was associated with a decline of 2.79 points on the HAM-A scale while also being among the best tolerated drugs included.
Of the new drugs, only agomelatine seemed to be effective in reducing symptoms, with an effect size nearly as strong as that of quetiapine, however, tolerability of this drug is unclear at this stage.
Finally, ocinaplon showed promising results with a large reduction in symptoms of 7.9 points. However, this estimate was based on a limited sample and as such, further research into the use of this drug is warranted.

This huge review suggests that there are several effective treatment choices for generalised anxiety disorder across classes of medication.
Conclusions
- Through their analyses, the authors concluded that there are several pharmacological options for the treatment of generalised anxiety disorder, some slightly more effective than others with varying patterns of tolerability.
- Treatment decisions should therefore be guided by the individual with the aim of finding the best fit in terms of efficacy, tolerability, and side-effect profiles.
- This research also guides future researchers in terms of promising treatments for which further evidence is required.

According to this review, Venlafaxine, Pregabalin, Escitalopram, and Duloxetine are viable alternatives to traditional drug treatment for generalised anxiety disorder.
Strengths
Possibly the largest contemporary review of pharmacological drugs available for the treatment of generalised anxiety disorder, this study holds novelty in terms of sheer scale and size. The study is further strengthened by facilitating comparisons between newer treatments and drugs like benzodiazepines. Moreover, by consistently measuring efficacy and acceptability, the study provided updated and reliable evidence to clinicians about the newer drugs as compared to the existing options.
Limitations
The researchers acknowledged that the trials included were assumed to be similar despite having been conducted in a range of settings and some of them lacked clear details about their randomisation methods. Moreover, the study exclusively looked at comparisons in pharmacological treatments for generalised anxiety disorder while ignoring potentially effective non-pharmacological treatments such as cognitive-behaviour therapy (something perhaps for a future review?).
Finally, publication bias was a concern as most of the relevant RCTs were conducted by pharmaceutical companies as part of clinical development programmes. However, the researchers attempted to account for this by referring to multiple credible sources to identify the trials and through the inclusion of non-English language and unpublished studies.
Implications
The study substantiates clinical evidence for drugs like Venlafaxine, Pregabalin, Escitalopram, and Duloxetine as viable alternatives to Benzodiazepines and other classic drugs for the treatment of generalised anxiety disorder (GAD). Moreover, by measuring the efficacy and acceptability of the different drugs, the study provides evidence for drugs that may be used as second-line treatments, drugs that may not be effective at all or may be effective in only certain regions of the world (e.g. Mirtazapine seen to be effective only in China). Thus, the study provides clinically relevant information that can be used by clinicians and NICE guidelines to prescribe and suggest appropriate pharmacological recommendations for the treatment of GAD.
With respect to implications for research, the study brings to light new sources of information such as online clinical registries that facilitate inclusion of unpublished studies and earlier-phase trials, which are otherwise inaccessible. Furthermore, inclusion of commercially sensitive and unpublished studies enables more holistic and representative analyses and comparisons of different interventions, thereby leading to a more robust study.
Finally, by referring to international databases such as the Chinese National Knowledge Infrastructure (CNKI), this study has opened doors for more trials to be included in future network meta-analyses and research, thus allowing better opportunities for the comparison of direct and indirect evidence.
The reviewers argue that initial failure of drug therapy for generalised anxiety disorder might not be a reason to abandon medication, and suggest that second-line treatments should be considered.
Contributors
Thanks to the UCL Mental Health MSc students who wrote this blog: Vicky Bamber (@vbambr), Aakanksha Kumar, Georgia Penska (@georgia_penska), Natalie Wong (@nat2w), Dylan Peters (@dylan_peters1), Taarika Chugh (@taarikac), Noor Hassan (@Noor0396), Dawn Wong (@dawnwongyh), Vanessa Daccach (@vanessadaccach), Robyn Feldman (@robynfeldman1).
Conflicts of interest
None.
UCL MSc in Mental Health Studies
This blog has been written by a group of students on the Clinical Mental Health Sciences MSc at University College London. A full list of blogs by UCL MSc students from can be found here, and you can follow the Mental Health Studies MSc team on Twitter.
We regularly publish blogs written by individual students or groups of students studying at universities that subscribe to the National Elf Service. Contact us if you’d like to find out more about how this could work for your university.
Links
Primary paper
Slee et al (2019). Pharmacological treatments for generalised anxiety disorder: a systematic review and network meta-analysis. The Lancet https://doi.org/10.1016/S0140-6736(18)31793-8
Other references
Bandelow B, Reitt M, Röver C, Michaelis S, Görlich Y, Wedekind D. Efficacy of treatments for anxiety disorders: a meta-analysis. Int Clin Psychopharmacol 2015; 30: 183–92.
Baldwin DS, Waldman S, Allgulander C. Evidence-based pharmacological treatment of generalized anxiety disorder. Int J Neuropsychopharmacol 2011; 14: 697–710.
Faltinsen, E., Storebø, O., Jakobsen, J., Boesen, K., Lange, T., & Gluud, C. (2018). Network meta-analysis: the highest level of medical evidence?. BMJ Evidence-Based Medicine, 23(2), 56-59. doi: 10.1136/bmjebm-2017-110887.
Hoge, E.A., Ivkovic, A., & Fricchione, G.L. (2012). Generalized anxiety disorder: diagnosis and treatment. BMJ, 345(27). doi: 10.1136/bmj.e7500.
National Institute of Health and Care Excellence. (2011). Generalised anxiety disorder and panic disorder in adults: management (Clinical guideline CG113). Retrieved from https://www.nice.org.uk/guidance/cg113.

Pregabalin is an increasingly popular drug of abuse. https://emj.bmj.com/content/30/10/874.2
thanks – helpful