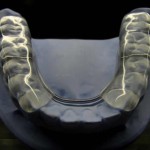
A number of treatment options are available for the management of painful temporomandibular disorders. These include counselling, physiotherapy, pharmacologic treatment, behavioural medicine, including acupuncture, transcutaneous electrical nerve stimulation (TENS) and occlusal appliances. Stabilisation appliances, in particular the Michigan splint are the most commonly used occlusal appliances although the mechanism of action is unclear.
The aim of this review was to assess the efficacy of stabilisation appliances in the management of painful temporomandibular disorders (TMDs).
Methods
Searches were conducted in the Medline, Embase, CINAHL, Cochrane Central Registry of Controlled Trials (CENTRAL), and Scopus databases. Randomised controlled trials (RCTs) in adults with myogenous, arthrogenous, or mixed TMD pain (classified on Research Diagnostic Criteria for TMD (RDC/TMD) or the Diagnostic Criteria for TMD (DC/TMD) comparing complete-coverage flat hard or resilient with an active or passive placebo appliance were considered. The primary outcome was pain intensity scores using a visual analogue scale (VAS). Two reviewers independently extracted data and assessed the risk of bias using the Cochrane tool. Mean difference was used to analyse via frequentist network meta-analysis.
Results
- 24 RCTs were included.
- 11 RCTs (508 patients) evaluated pain intensity and 16 RCTs (679 patients) pain improvement.
- 7 studies were considered to have a low risk of bias, 12 an unclear risk and 5 a high risk.
Pain Intensity
- SA v non-occluding appliances (6 RCTs) no significant difference; MD= -0.502 (95%CI; -1.322 to 0.318).
- SA v untreated controls (5 RCTs) showed a significant reduction in pain in- tensity when compared with the untreated controls; MD= -2.03, (95%CI; – 2.7 to -1.2)
- The network meta-analysis (NMA) included 11 RCTs, 508 participants, and 3 comparisons and showed Pain at follow-ups was: –
- Significantly higher in the untreated control group when compared with SA; MD = 2.04, (95%CI;1.26 to 2.8).
- Reduced but not significantly, by treatment with SA compared with non-occluding appliances; SM = 0.50 (95%CI; -0.26 to 1.26).
- Significantly reduced after treatment with non-occluding appliances when compared with untreated controls; DM = -1.54 (95%CI; -2.6 to -4.6).
Pain Improvement
- Meta-analysis showed a significantly higher number of participants reporting pain improvement after treatment with SA compared to treatment with:-
- Non-occluding appliances; RR (Risk Ratio) = 1.37 (95%CI; 1.15 to 1.64) and
- Untreated controls; RR = 1.51; CI: 1.16 to 1.98).
- The NMA (11 RCTs) showed a significantly higher number of participants reporting pain improvement after treatment with SA when compared with:-
- Non-occluding appliances; RR=0.70 (95%CI; 0.52 to 0.92) and
- Untreated controls (low-quality evidence; RR=0.55; CI: 0.35 to 0.86).
- The NMA found no statistical difference in number of participants reporting pain improvement between after treatment with non-occluding appliances and with untreated controls; RR = 1.29 (95%CI; 0.75 to 2.2).
Conclusions
The authors concluded: –
This network meta-analysis showed no significant difference in reported pain intensity at follow-ups between the treatment of painful TMDs with stabilisation appliances or non-occluding appliances (active placebo). However, a significant difference in participants reporting treatment satisfaction with reduced pain, and a significantly lower number needed to treat in favour of stabilisation appliances were found. Patient-reported treatment satisfaction probably included more domains than just pain intensity, such as improvements in physical functioning and psychosocial factors, and deserves further investigation. The authors concluded that stabilisation appliances treatment efficacy is beyond the placebo effect.
Comments
This review seeks to determine whether the efficacy of a stabilisation appliance in managing painful TMDs was greater than any placebo effect. The authors have compared the stabilisation appliance (i.e one with, a flat, smooth surface in polymethyl methacrylate against the opposing teeth and can be designed with or without palatal coverage) with both active placebos (non-occluding appliances) and passive placebos (untreated controls). While 24 RCTs were included in the review the numbers contributing to the various meta-analyses conducted was smaller. There was also variation in clinical and methodological aspects of the included studies which is consistent with an earlier review of occlusal splints for TMDs (Dental Elf – 20th Jul 2020). Agreement on a set of common outcome sets for future TMD studies would be helpful both to improve the consistence and quality of future studies and reviews.
Links
Primary Paper
Alkhutari AS, Alyahya A, Rodrigues Conti PC, Christidis N, Al-Moraissi EA. Is the therapeutic effect of occlusal stabilization appliances more than just placebo effect in the management of painful temporomandibular disorders? A network meta-analysis of randomized clinical trials. J Prosthet Dent. 2020 Oct 15:S0022-3913(20)30464-9. doi: 10.1016/j.prosdent.2020.08.015. Epub ahead of print. PMID: 33070972.
Other references
Dental Elf – 20th Jul 2020
Occlusal splints for the management of temporomandibular disorders
Dental Elf – 23rd Sep 2013
Review suggests that counselling may have a role in management of temporomandibular disorders
