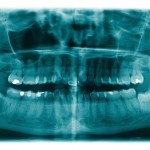
The surgical removal of lower third molars is a commonly undertaken procedure associated with pain swelling and trismus. Other complications include infection, alveolar osteitis, adjacent tooth damage and temporary or permanent nerve damage. Traditional approaches to managing pain. swelling and trismus include the use of analgesia, steroids and cryotherapy while recent studies have suggested potential benefits from the use of low-level laser therapy (LLLT).
The aim of this review was to assess whether low-level laser therapy (LLLT) is effective in reducing postoperative morbidity in patients undergoing surgical removal of mandibular third molars compared with placebo.
Methods
Searches were conducted in the Medline, Embase, Dentistry and Oral Sciences Source, Cumulative Index of Nursing and Allied Health Literature, Academic Search Complete, Cochrane Library, World Health Organization International Clinical Trials Registry Platform, www.ClinicalTrials.gov, www.controlledtrials.com OpenGrey and Google Scholar databases. This was supplements by hand searches of the Journal of American Dental Association, International Journal of Oral and Maxillofacial Surgery, British Journal of Oral and Maxillofacial Surgery. Randomised controlled trials (RCTs) comparing treatment group of LLLT with a placebo control group were considered. Two reviewers independently selected studies, extracted data and assessed risk of bias using the Cochrane tool. The main outcomes were postoperative pain, swelling, and trismus. Meta-analyses were conducted using a random-effects model.
Results
- 17 RCTs (9 Split-mouth, 8 Parallel) involving 1064 patients were included.
- Type of LLLT used, approach, power, site and duration of application varied across the studies.
- Co-interventions included antibiotics (9 studies), acetaminophen (7 studies), NSAIDs (6 studies).
- 8 studies were at high risk of bias in at least one domain, 7 at unclear risk and 2 at low risk.
- 15 studies measured pain with 5 studies contributing to a meta-analysis which showed a non-significant reduction on day 2 and 7 compared with control: –
- SMD (2 days) = -502 (95%CI; -1.038 to 0.03).
- SMD (7 days) = -0.244 (95%CI; -0.542 to 0.53).
- 11 studies considered swelling with 5 studies contributing to a meta-analysis demonstrating significant reductions in swelling at day 2 and day 7 postoperatively
- SMD (2 days) = -0.661 (95%CI; -0.988 to -0.234).
- SMD (7 days) = -0.532 (95%CI; -0.795 to -0.269).
- 11 studies considered trismus with 6 studies contributing to a meta-analysis which showed a non-significant reduction on day 2 and 7 compared with control: –
- SMD (2 days) = 0.002 (95%CI; -1.159 to 1.163).
- SMD (7 days) = 0.075 (95%CI; -1.187 to 1.036).
Conclusions
The authors concluded: –
LLLT significantly reduces swelling after extraction of mandibular third molars compared with placebo. LLLT has not shown to reduce postoperative pain and trismus. LLLT does not cause adverse effects. There is currently insufficient evidence available, to promote the investment in LLLT vs the net clinical benefit. Randomized controlled trials with larger sample size and standardized study design and outcome measures are required, to make definitive recommendations to clinicians on its use on patients.
Comments
The authors preregistered the review protocol on PROSPERO and have undertaken and extensive search. While a good number of RCTs (17) have been identified they are mainly small in size and of limited quality with a majority (8) being at high risk of bias in at least one domain. The authors highlight clinical and methodological heterogeneity between the included studies with variation in the type and power of LLLT used, site and duration of application. They also indicate that a number of the studies also included co-interventions and it would have been helpful for more information to have been provided on this.
Several meta-analyses were conducted in relation to pain, swelling and trismus although only a small number of the homogeneous contributed with a statistically significant benefit being demonstrated for swelling only. The authors indicated that while a statistically significant benefit was shown there remains debate as to whether this is of any clinical significance. We had previously looked at a review of this topic in 2012 (Dental Elf – 13th Apr 2012) and that was updated in 2017 ( Dawdy et al.2017 ) who concluded:-
LLT probably has negligible benefits but may not result in adverse events. Evidence does not support the use of LLLT in clinical practice to reduce complications after impacted mandibular third-molar surgical extractions.
While a number of new studies have been published since 2017 they are insufficient to add additional clarification regarding the use of LLLT in lower third molar surgery.
Links
Primary Paper
Domah F, Shah R, Nurmatov UB, Tagiyeva N. The Use of Low-Level Laser Therapy to Reduce Postoperative Morbidity After Third Molar Surgery: A Systematic Review and Meta-Analysis. J Oral Maxillofac Surg. 2021 Feb;79(2):313.e1-313.e19. doi: 10.1016/j.joms.2020.09.018. Epub 2020 Sep 17. PMID: 33058775.
Other references
Dental Elf – 13th Apr 2012
Dawdy J, Halladay J, Carrasco-Labra A, Araya I, Yanine N, Brignardello-Petersen R. Efficacy of adjuvant laser therapy in reducing postsurgical complications after the removal of impacted mandibular third molars: A systematic review update and meta-analysis. J Am Dent Assoc. 2017 Dec;148(12):887-902.e4. doi: 10.1016/j.adaj.2017.06.043. Epub 2017 Oct 5. PMID: 28987483.
