Randomised controlled trials (RCTs) are widely regarded as the gold standard study design for assessing the efficacy and safety of a treatment. However, they are voluntary and rely on people adhering to their treatment. Furthermore, measuring hospitalisation and mortality outcomes is only possible with thousands of patients in long expensive studies. Considering the cohort of patients (people with a diagnosis of schizophrenia), an RCT like this may be practically impossible to do.
Even if you could perform this study, it may not actually represent most patients; up to 90% of patients are excluded because of refusal, substance abuse, suicidal/antisocial behaviour or mental/physical comorbidity.
Short term RCTs tell us that clozapine, olanzapine and amisulpride are better than other antipsychotics but in the long term, typical and atypical antipsychotics have similar efficacy and three quarters of patients will need to change their treatment within 18 months (Lieberman et al, 2005). We also do not know how depot injections compare to oral treatments in general and between different antipsychotics.
A real-world observational study has overcome the typical difficulties with RCTs in a nationwide study of electronic databases of hospitalisation, mortality and dispensed prescriptions involving schizophrenia patients in Sweden (n=29,823, including 4,603 newly diagnosed patients, data collected from 1 July 2006 to 31 December 2013) (Tiihonen et al, 2017).

“Difficult” patients are often excluded from randomised controlled trials, making the findings much more challenging to use in the real-world.
Methods
What makes this analysis unique is that outcomes were compared for patients when they were on medication vs. when they were off medication. Hence, each patient acts as their own control, effectively eliminating patient-specific confounding factors and selection bias, without the need to statistically adjust for these. Antipsychotic effectiveness was compared while adjusting for time receiving monotherapy only and time receiving any therapy.
Treatment failure was defined as discontinuation or switch of antipsychotic medication.
Results
43.7% of patients experienced psychiatric hospitalisation and 71.7% had treatment failure. The mean duration of follow-up in the total cohort was 5.7 years (median, 6.9 years). Oral olanzapine was the most frequently used drug and zuclopenthixol the most frequently used depot.
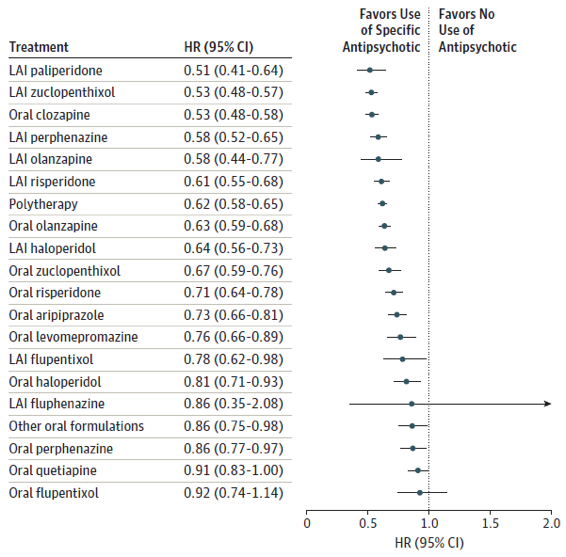
Using antipsychotics vs not using antipsychotics: risk of hospitalisation
The risk of hospitalisation was lower with all antipsychotics, except oral quetiapine, depot fluphenazine and oral flupentixol.
Antipsychotics vs Olanzapine: risk of hospitalisation
All depot injections were significantly better than oral olanzapine, except depot fluphenazine. However, oral olanzapine was not worse than other oral antipsychotics, apart from clozapine.
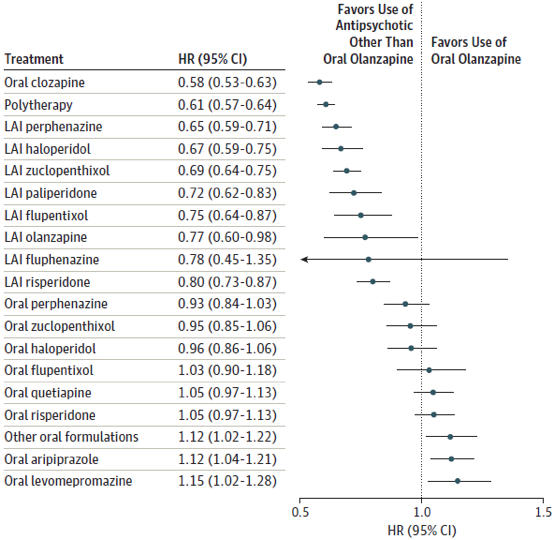
Significantly better treatments than oral olanzapine at reducing the risk of hospitalisation (p<0.001 for all comparisons)
Oral clozapine, Depot perphenazine, Depot haloperidol, Depot zuclopenthixol, Depot paliperidone, Depot flupentixol, Depot risperidone
LAI: long acting injectable (depot), HR: hazard ratio, CI: confidence interval
Depot vs oral
Rehospitalisation was 22% less likely with depot antipsychotics compared with using the corresponding oral formulations (HR 0.78; 95% CI 0.72 to 0.84; p<0.001).
Treatment failure
The lowest risk of treatment failure was observed for clozapine (HR 0.58; 95% CI 0.53 to 0.63), followed by depot injections (HRs; 95% CI 0.65 to 0.80) and highest with levomepromazine (HR 1.15; 95% CI 1.02 to 1.28).
None of the results were influenced by the use of concomitant antidepressants or benzodiazepines.
Newly diagnosed cohort
In the newly diagnosed cohort, the risk of psychiatric rehospitalisation was 32% lower during treatment with depot injections compared with treatment with equivalent oral formulations (HR, 0.68; 95% CI 0.53 to 0.86). Hence, use of depot antipsychotic medications results in the greatest benefit during the early phase of the illness

These results suggest substantial real-world differences between specific antipsychotic agents and between routes of administration.
Comment
All in all, this shows that patients should be offered depot injections as first line treatment, not wait for the disease to progress. Let me explain:
When I write these blogs, I always try to think from the clinician’s perspective: Are these findings applicable to my patient group? Can I implement any changes? Is this just an interesting read and nothing more?
This is more than just an interesting read. We have solid data on hard outcomes for a group of drugs that have needed this for years. Not surprisingly, clozapine performed consistently, as did depot injections, they were substantially more effective than other antipsychotics in reducing the risk of rehospitalisation or any treatment failure. As we cannot use clozapine as first line treatment, therefore, patients should be switched to depots as soon as patients respond to their oral counterparts and can tolerate treatment, well before they get worse.
If I had to guess, I would say that the key is medication adherence, equally, it might be the regular contact with medical staff necessitated by blood samples and injections. The increased costs of regular contact with psychiatric patients is almost definitely offset by reduced hospitalisation and treatment failure. Even if it is not offset, one could argue that this is a price worth paying to keep this group of people out of hospitals so that they may lead normal lives.
On the other end of the spectrum we have quetiapine performing consistently poorly. Based on these results alone, it seems quetiapine should be reserved as adjunct treatment. However, its use may be focused in patients with negative schizophrenia symptoms, which are notoriously difficult to treat.

Does this real-world evidence justify the use of depot antipsychotics as first line treatment for schizophrenia? Share your thoughts below and on Twitter.
Strengths and limitations
Being a nationwide study based on medical records, it would be safe to assume there is no missing data (in RCTs, the dropout rates are 50% to 60% and higher in oral antipsychotic RCTs).
It would be useful to have an overview of some ‘soft outcomes’ like symptom control, adverse effects and quality of life. However, they are of secondary importance to the bigger questions answered by this study.
No data were available for concomitant psychological treatment, on the use of mood stabilisers or the influence of race on the outcomes. With regards to race, the results from this Swedish study can be generalised to Caucasians but may not necessarily apply to those of other ethnicities, who have higher rates of psychiatric illness, compared to Caucasians.

This study does not include information on symptom control, adverse effects or quality of life. Does this matter?
Links
Primary paper
Tiihonen J et al. (2017) Real-World Effectiveness of Antipsychotic Treatments in a Nationwide Cohort of 29 823 Patients With Schizophrenia. JAMA Psychiatry. 2017;74(7):686-693
Other references
Lieberman JA et al. (2005) Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209-23

Interested in recovery and QOL outcomes.
Are these measured in the paper. Also health risks and early deaths?
Hi Ben
The paper only looked at hard endpoints; hospitalisation rates and treatment failure
DID IT CONSIDER THE MISERY PEOPLE WERE LIVING IN BEING CHEMICALY COSHED WITH NO QUALITY OF LIFE? DID IT CONSIDER ALL THE LONG AND SHORT TERM EFFECTS, EG, MORE ILLNESSES, SHORTENED LIFE SPAN OR INDEED SUICIDE, OR THE HARM CAUSED TO OTHERS? IT IS ABOUT TIME THAT THE OVERALL PICTURE WAS PORTRAYED AND NOT THE ONE THE PHARMACEUTICAL COMPANIES WISH TO PORTRAY TO CONTINUE MAKING MONEY AT THE EXPENSE OF LIVES! ADERHOLD & STASTNY GUIDE TO MINIMUM USE OF NEUROLEPTICS SAYS IT ALL AND THANKFULLY PANORAMA HAS OPENED UP A HORNETS NEST THAT NEEDS FURTHER EXPLORATION. PSYCHIATRICT MEDICATIONS HAVE BEEN ALLOWED TO BE PRESCRIBED UNDER DISPROVEN HYPOTHESES CAUSING MUCH HARM TO MANY, SOME LIVES YOU CANNOT BRING BACK, PSYCHIATRY NEEDS A COMPLETE OVERHAUL AND I HOPE THE LIKES OF PANORAMA WILL HELP IT ON ITS WAY!
Yes
This could have interesting implications for those with schizo affective disorder and bipolar 1.