
Individuals with autism spectrum conditions (ASC) typically present difficulties in three main areas: social interaction, communication and imagination, and may also display repetitive and stereotyped behaviours which can cause self-injury (NAS, 2015).
There are many theories about what causes these core behaviour symptoms in individuals with autism spectrum conditions, in particularly self-injurious behaviour (SIB). One hypothesis is that there is an issue in the opioid brain system where striatal beta endorphins which create emotional ‘highs’ (Research Autism, 2015) have failed to reduce with maturation. Engagement in SIB is thought to release these endorphins which block any pain and provide a feeling of euphoria (Edelson, 2015).
This hypothesis has been somewhat supported by studies which have found that opioid antagonist drugs which block endorphins can ameliorate such behaviours; however conclusions about their efficacy are mixed (Lewis, 1996). One type of opioid antagonist drug, Naltrexone, has been previously used in the management of children with ASC and has shown significant reductions in SIB.
This paper reviews 10 studies that have tested Naltrexone with children with autism spectrum conditions.
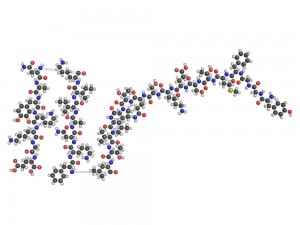
Opioid antagonist drugs like Naltrexone are thought to prevent the body’s response to endorphins
Method
The authors systematically reviewed the available evidence on Naltrexone, examining whether those who took this medication showed improved behaviour and/or any side effects.
The collection of the articles involved 4 elements: the search of four electronic databases; the cross-referencing of relevant reviews; a hand search of papers in any of the major international intellectual disability journals for papers (between 2010 and 2012), and an unpublished clinical trials search. Each database was searched up to 2013.
The authors used a wide-range of search terms for intellectual disability, autism spectrum disorder, opioid antagonists, and other specific drugs.
A total of 866 citations were generated prior to filtering. Papers were filtered firstly by titles (712 excluded), abstracts (78 excluded) and then full-texts (56 excluded). The remaining 20 papers were split into 10 studies on adolescents and adults, and 10 on children which are reported on in this paper.
Full texts were scrutinised using a pre-designed inclusion criteria by two independent reviewers. Their decisions were then discussed with the study group. The inclusion criteria included:
- Randomised control trials (RCTs)
- Participants (adults and children for the overall study) of any age with an IQ below 70 who exhibited problem behaviour (PB)
- Studies where there were participants with and without intellectual disability, including those with or without autism spectrum disorder
- Symptoms – any behaviour problem or a symptom related to ASC
- Any orally taken opioid antagonist which had been prescribed for the management of problem behaviour (excluding the drug Naloxone)
- Outcome measure where there was a pre and post intervention (these included behavioural measures and measures of side effects)
- Papers written within any year or type of publication (including book chapters and conference proceedings)
As well as measuring the content of the papers and their adherence to the inclusion criteria, the authors reviewed the quality of the RCTs.
Findings
- 155 children participated in the 10 studies, with 27 of these children receiving a placebo drug
- 7 of the studies were conducted with outpatients, with a third of participants in the remaining 3 studies also outpatients
- The number of participants in each study varied from 4 to 41
- 125 of the participants were boys, 30 were girls
- All the children had a diagnosis of ASC but the level of intellectual disability varied greatly. Some participants were non-verbal
- Some studies reported that children had comorbid conditions (e.g. Down syndrome, epilepsy)
- Children were also taking different types of medication. Some studies reported that this medication had been temporally stopped during the trial period, whereas in others they had continued to take it, or had not provided details
Key findings:
- 98 out of the 128 children (77%) in the 10 studies that received the drug Naltrexone had a statistically significant improvement in symptoms of irritability and hyperactivity.
- Overall the drug was well-tolerated with very mild side effects. The authors did however comment that naltrexone has a bitter taste and was thus difficult to administer.

Naltrexone improved symptoms of irritability and hyperactivity in 77% of children but was not effective in improving the overall core features of ASC
Conclusion
While the review found that Naltrexone had a significant effect in 77% of children, the authors are cautious given the small number of studies and that it did not have an impact on the core features of ASC within the majority of children.
Strengths and limitations
The review effectively analyses the evidence on opioid antagonists with children with ASC. The authors begin by usefully introducing the state of the work on opioid antagonists and how this leads to their own meta-analysis which reviews papers up until 2013. While the papers they reviewed are no longer as current, 2013 is when the process of the review was conducted and it effectively assesses the utility of naltrexone and suggests further avenues for research.
The authors provided a clear yet detailed account about how they went about the meta-analysis. The procedure they took in selecting and filtering the articles appears to be methodical, graduated and thorough, with reasons provided for discarded articles. The use of two independent reviewers plus a study group to review decisions also demonstrates the rigour of the review. Meticulous detail was provided about where the articles were obtained from and their inclusion/exclusion criteria were clearly presented.
The use of tables to break down the components of each study and the flow diagram demonstrating their filtering procedure are helpful additions that guide readers through their process.
One possible criticism of the inclusion/exclusion criteria is that in some cases these were very broad, which could increase variability when ascertaining whether the drug works. For example, there were no restrictions on target symptoms as long as they were a behavioural problem or symptom of ASC, and any outcome measure could be used as long as they had pre- and post- results.
However, it is important to recognise that the collation of results from many different studies is a challenge due to the use of different participants and outcome variables, and given that there were only 10 studies with children that fit the final criteria, narrowing-down further would have decreased its scope.
More importantly in practice, to exclude certain behaviours and outcomes would be a mistake given that children on the autistic spectrum are incredibly diverse.
The summary at the end of the paper succinctly presents the findings and what they mean for future research, however a short discussion about the implications of the results for practice would have been a useful addition. Could it be that the future treatment of children with ASC takes more of a medical, pharmacological focus?
Will there still be a role for behavioural interventions? Given the findings of this paper it appears that this will depend on the behavioural symptoms that a child is presenting and their current treatment and support. Similar to behavioural programmes, not one intervention fits all, and therefore the ability of opioid antagonist drugs to attenuate the core symptoms of ASC in children will need to be evaluated on a case-by-case basis.
Summary
Based on a review of 10 papers, the authors have found that the opioid antagonist drug Naltrexone can reduce irritability and hyperactivity in 77% of children. Nevertheless, they are rightly cautious about these results given that the drug did not reduce the core symptoms of ASC.
With such diversity both in terms of the population of those with ASC and the study sample (for example different target symptoms, outcomes, behaviours, comorbidity and medication usage), it is especially difficult to find something that suits all. Particularly when there is a focus on children, it is exceptionally difficult to ascertain whether any improvement is due to the drug, short-term fluctuation, a child’s developmental trajectory, or something else altogether.
To conclude, it is sensible that the authors advocate for further research to look more closely at the subgroup of children who did respond well to naltrexone. However it is also important to consider that in practice a child’s problem behaviour will be assessed and supported on an individual basis which could involve a combination of medication and intervention.

Treatment and support of children with ASC will always need to be tailored to the individual
Links
Roy, A., Roy, M., Deb, S., & Unwin, G. (2015). Are opioid antagonists effective in attenuating the core symptoms of autism spectrum conditions in children: a systematic review. Journal of Intellectual Disability Research, 59(4), 293-30 [abstract]
Edelson, S. M. (2015). Understanding and treating self-injurious behaviour. Retrieved 09.05.15
Lewis, M. (1996). Brief report: Psychopharmacology of autism spectrum disorders. Journal of Autism and Developmental Disorders, 26(2), 231-235
NAS. (2015). Recognising autism spectrum disorder. Retrieved 09.05.15
Research Autism. (2015). Opioid antagonists and autism. Retrieved 09.05.15

@LearningDisElf the page isn’t found when I click on the link
@Kl3io apologies. try http://t.co/Tm8EjNDQJq
@LearningDisElf TY this link works.
Does opioid antagonist medication improve the core features of autism spectrum conditions in children? http://t.co/ad8dQUScls
My latest review for the @LearningDisElf, take a look: http://t.co/TlXlF2mGxt #autism #treatment
Treatment and support of children with autism spectrum conditions need to be tailored to the individual http://t.co/ad8dQUScls
@LearningDisElf totally agree, but what does government suggest https://t.co/r0Y9IXLUTL Not good, dylan hartley as a role model then!
Does opioid antagonist medication improve the core features of autism spectrum conditions in children?… http://t.co/oQlx8xWLgG
Don’t miss: Does opioid antagonist medication help core features of autism spectrum conditions in children? http://t.co/ad8dQUScls #EBP
http://t.co/A5E0mPEYAS… http://t.co/2se1Zt5F3V
RT @autismcornwall: Do opioid antagonist meds improve core features of #autism spectrum conditions in kids? http://t.co/SCTBQZVxsr