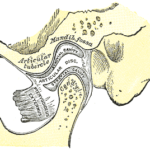
Temporomandibular disorders (TMD) include degenerative conditions of the articulating surfaces of the temporomandibular joint (TMJ). Of these osteoarthritis (OA) is the most common affecting 8-9% of the population but up to 55.6% of those with TMD. Management of degenerative TMD focuses on alleviating the functional pain and establishing normal range of mandibular movements. Non-invasive treatments are the first line of management but intra-articular injections of hyaluronic acid (HA) have shown positive effects. Platelet-rich plasma (PRP) a concentrate of platelets from the patient’s blood and recently intra-articular injections of PRP have used for TMD.
The aim of this review was to determine the effectiveness of intra-articular PRP injections in patients with TMD compared to other treatments, such as injections of HA or saline.
Methods
Searches were conducted in the Medline and Scopus databases supplemented by a hand-search of relevant journals and the reference lists of selected articles. Randomised controlled trials (RCTs) in patients diagnosed with TMJ-OA receiving intra-articular injections of PRP or plasma rich in growth factors (PRGF) after arthrocentesis or arthroscopy, compared with controls receiving intra-articular injections of HA or saline or Ringer’s lactate solution after arthrocentesis or arthroscopy were considered. The primary outcomes were maximum mouth opening (MMO, in millimetres) and pain intensity. The risk of bias was assessed independently by 2 reviewers using the Cochrane Collaboration tool in the areas of selection bias, performance bias, detection bias, attrition bias, reporting bias, and other biases with the quality of the studies included being assessed using the Jadad scale. A narrative summary was presented
Results
- 6 RCTs involving a total of 323 patients were included.
- All 6 studies were at high risk of bias.
- 3 studies compared PRP with HA, 3 compared PRP with Ringer’s lactate or saline.
- 4 studies found PRP injections to be superior in terms of improvements in mandibular range of motion and pain intensity up to 12 months after treatment,
- 2 studies found similar results for the different treatments
Conclusions
The authors concluded: –
There is slight evidence for the potential benefits of intra-articular injections of PRP in patients with TMJ-OA. However, a standardized protocol for PRP preparation and application needs to be established.
Comments
The search strategy for this review is limited to 2 databases and publications in English so relevant studies may have been excluded. Only a small number of studies were identified, and all of the studies were at high risk of bias in particular because none of them included the blinding of the outcome assessor which raise important concerns regarding detection bias. There are also concerns relating to the blinding of the participants and personnel. In addition there are concerns regarding the efficacy of HA in the management of TMJ-OA for while an earlier review by Goiato et al (Dental Elf -29th Jul 2016) suggested it was beneficial, the review only included a small number of short term RCTs.
While the authors have suggested there is slight evidence for a benefit of PRP in the management of TMD it is better characterised as very weak. It is clear that high quality and well reported RCTs of appropriate size are needed to provide greater clarity on the broad range of invasive interventions currently being used for the management of TMDs.
Links
Primary Paper
Bousnaki M, Bakopoulou A, Koidis P. Platelet-rich plasma for the therapeutic management of temporomandibular joint disorders: a systematic review. Int J Oral Maxillofac Surg. 2018 Feb;47(2):188-198. doi: 10.1016/j.ijom.2017.09.014. Epub 2017 Oct 20. Review. PubMed PMID: 29066000.
Other references
Detection bias – Catalogue of bias
Dental Elf -29th Jul 2016
Temporomandibular joint arthrocentesis with hyaluronic acid- evidence limited.
Picture Credits

[…] post Temporomandibular disorders: Are intra-articular injections with platelet-rich plasma effective? appeared first on National Elf […]