
Down in the woodland the elves are all getting over the Christmas and New Year period. Too many magical baubles have been consumed, the tinsel has gone limp and the joy of the festivities has been replaced by the harrowing memory of being served a turkey for Christmas lunch! You humans are weird!
It’s time to turn our attention to more mundane things, and what better way to start 2023 with a bang than looking at this scoping review from Ledden et al. (2022) (and et al is doing a lot of heavy lifting in that sentence, there are loads of them).
‘Personality disorder’ is a contentious diagnosis. As this paper points out, its validity as a diagnosis is questioned and the diagnosis seems to come with multiple harms. Figures vary but around 5% of the population would meet the criteria for personality disorder, although around 50% of people in psychiatric outpatients and 70% of inpatients will have that label (Evans et al 2017).
There’s a general sense that people who are given a ‘personality disorder’ diagnosis experience stigma and discrimination, which results in a lack of care provision. Over the past 20 years, NICE guidelines (NICE 2009) have encouraged the formation of specialist services, but we can wonder whether these specialist teams have actually increased the quality of care on offer, or just given teams an excuse to say: “not my job, we’ll refer on to the specialists”.
This paper looks at the evidence for community provision (Ledden et al, 2022).

This new scoping review by Leiden et al (2022) explores community provision of ‘personality disorder’ services.
Methods
Now it’s in this section that we always feel absolute frauds. We shall throw glitter and sing elf songs to disguise our lack of expertise, but…
The authors did a search for community interventions that were primarily about ‘personality disorder’ or something that might fall into that wide and murky area, e.g. self-harm, emotional dysregulation. Papers had to study adults, include a particular treatment, approach or service model and any comparator was considered from RCTs to pre/post measures. Pretty much any outcome measure was included and all the studies were quantitative.
They describe a pretty robust process for selecting the articles, which we’re not in a position to critique, but it sounds so tedious and laborious that it must have been good.
Results
All the above whittled down 17,000 database results to 226 papers reporting on 210 studies. Six studies were done in Asia, the rest in western countries. CBT (cognitive behavioural therapy) and DBT (dialectical behaviour therapy) were the most researched interventions. No one was doing any studies in this area in the 1990s (a lack of research and a conviction that people couldn’t be helped. Any correlation there?), but things have improved since then. ‘Borderline Personality Disorder’ was the most studied diagnosis and unsurprisingly, most participants were White females.
There was evidence to support specialist approaches, but other things such as self-management, peer support or just “what does good support look like” weren’t really looked at.
Most of the evidence is about which 3 letter therapy is best. They’re all about as good as each other and all are better than “treatment as usual” (and treatment as usual can have some pretty dark implications for this group of people, in our experience it can often involve sitting on a clinic list in a CMHT while consuming polypharmacy).
Studies show that help helps. Various outcome measures were used, but things like diagnostic criteria were no longer met, and self-harm reduced etc.

This review found that help helps. Various therapies (e.g. CBT or DBT) were found to be about as effective as each other, and all were better than treatment as usual.
Conclusions
Service users and clinicians report that mental health care systems appear ill-equipped to deliver accessible care of high quality yet there are hardly any published investigations of the best approaches to designing teams and systems.
The authors highlight the dangers of unevaluated models of “care” being introduced, giving the example of Serenity Integrated Mentoring which attracted wide criticism (See this website for more details).
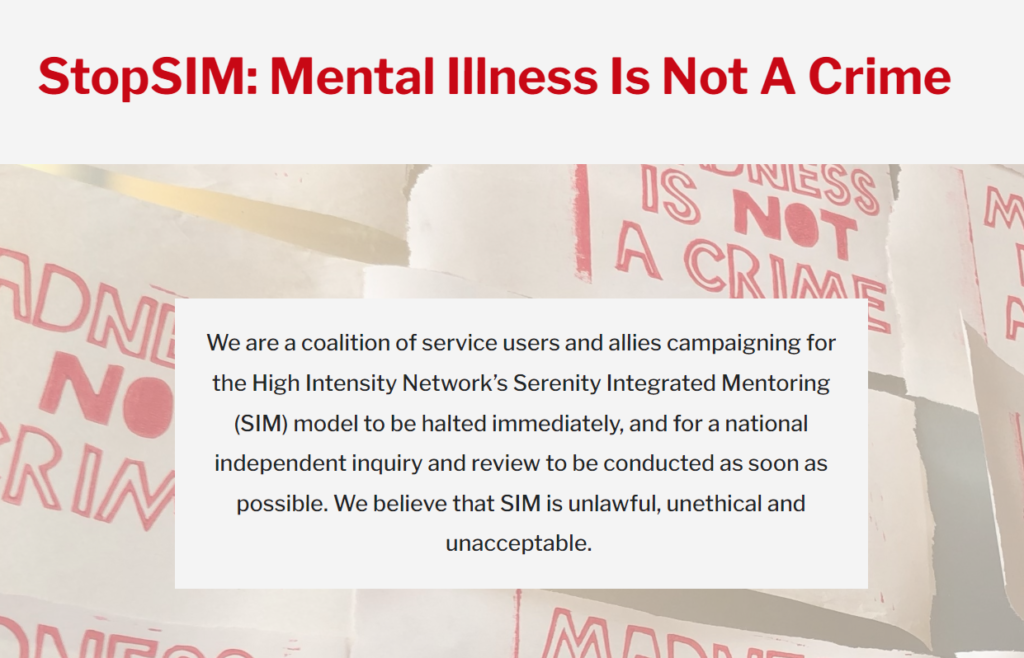
The authors highlight a concern over unevaluated models of care being introduced, such as the widely criticised SIM model.
Strengths and limitations
The search strategy was not peer reviewed and skipped anything not written in English, which limits the results to mainly Western cultures.
All of the papers were quantitative so while effects can be measured, we learn little about why the effects took place.
Purists might say that it didn’t focus purely on people meeting the criteria for ‘personality disorder’. Realists might say ‘personality disorder’ is a messy label that accommodates any person who self-harms, people with difficulties more likely explained as ASD, ADHD, Complex Trauma, PTSD or even just an understandable reaction to shitty life experiences and an iatrogenic care system. As a result, this scoping review looked at people who would typically attract a ‘personality disorder’ diagnosis, rather than people who really had a ‘personality disorder’ (which you can argue isn’t a valid or ethical way of describing people). Strength or weakness? You decide.
The team included lived experience researchers. The paper talks of the importance of doing this in research.
We can’t really skip over the fact that this paper by the Mental Health Policy Research Unit has opted to ditch the term ‘personality disorder’:
We are sympathetic to the critique that the therapeutic nihilism and stigma accompanying a “personality disorder” diagnosis, and the lack of progress in delivering care that consistently helps rather than harms, are such that this diagnostic label—also criticised on grounds of validity—is now best left behind.
Throughout the paper the term complex emotional needs is used instead and while it might not be perfect, we can at least celebrate a move away from describing someone’s personality as disordered. We suspect this change wouldn’t have happened without the presence of lived experience researchers on the team.
We’re both happy to celebrate people getting described in ways other than a disordered personality. The term complex emotional needs has skipped out of this paper and is becoming part of the service structure of different trusts across the UK. If used in the context of this paper as a catch all term for those who don’t respond well to medication, it seems ok, but our worry is that it becomes purely a euphemism for ‘personality disorder’. The name changes, but the services remain the same. People with PTSD, CPTSD and neurodivergence are either not part of the service, or included yet understood in terms of ‘personality disorder’. Our worry is that more people are understood in a stigmatised way, rather than a greater pool of people experiencing thoughtful, non pathologising formulation.
The resistance to telling adults and children that their personality is disordered is a very British phenomenon. This is a very political (and from our perspective laudible) decision, but may make the paper less accepted internationally.

The authors should be commended for their sensitive approach to ‘personality disorder’ which included ditching this term altogether and using ‘complex emotional needs’ instead.
Implications for practice
The implications of these findings might be less about practice and more about research. There is much that is not looked at. Studies tend to measure the things that frighten services (self-harm, bed use etc) and less of the things the paper describes as important to patients (relationships, employment, iatrogenic harm etc). We don’t know much about different populations and very little about minorities.
We might think 200 studies over 30 years is miniscule. There needs to be more of a focus on what works (or not) in generic care, or how services can be structured to be most useful. Critics might argue that 200 studies is poor, but try getting funding for studies without clear diagnostic criteria. This approach might mean that while the UK gets on with co-production and non-diagnostic approaches, the rest of the world will do the million pound RCT studies:
investment in large well-designed studies that test clear primary hypotheses has remained very limited around the world, which may reflect a continuing lack of optimism, and the impacts of the particularly severe stigma.
Let’s start shining lights in dark places as Sue Sibbald and Norman Lamb urged us to a few years back (Lamb et al 2020).

The review included 200 studies over 30 years, but more studies are needed. Particularly those that focus on what works in generic care and how services can be structured to be most useful.
Personal commentary
Outside of the constrains of the need to review the paper, we now move on to the stuff we are good at. Pure unsubstantiated opinion, delivered with passion and a good deal of table-thumping.
While this paper aims to explore what is and isn’t seen to be useful, one of our big questions is “useful to whom?”. The outcome measures used were nearly exclusively chosen by researchers and what matters to services may matter a lot less to patients.
Honestly, the idea that only specialist services can help is surely one of the most poisonous notions in mental health. Specialist services are like a little oasis in services in that they tend to attract people who want to work with a particular client group. We can wonder how much of the impact of specialist interventions is about patients working with those who have chosen to work with them.
We’ve also had the experience of specialist services being a dumping ground for people the CMHT didn’t want to work with. When you see how much this population benefits from placebo medication it’s clear that even a minor break from the norm can make a difference. How much of what is being measured as ‘beneficial’ is the thing being measured, and how much is a long-term, boundaried and thoughtful therapeutic relationship?
While we might celebrate the benefits ‘specialist’ interventions can bring, we know little about people’s return to secondary care and working with those who may not see themselves as having the skill or inclination to work with them. The move from a psychologically-informed approach to a generic service is quite the cliff edge to fall off and just as uncomfortable. The difference is that those who fall from cliffs are generally not blamed for the outcomes.
Our experience in the NHS was that the typical CMHT approach wasn’t that helpful for us or the clients we worked with. We sat in multidisciplinary teams where there was a reluctance to take the case of the person who was self-harming, we saw huge resistance to admission, we saw (perversely) even greater reluctance to discharge and a great passion for exporting traumatised young women to self-declared specialist units regardless of quality. We attempted to offer something resembling NICE recommended care in the community instead and of the last 5 people we worked with, they had 1,230 days in hospital before we got involved, and only 2 in the year after. We don’t think we offer anything that involves rocket science or brain surgery, but we think we might highlight how typical community mental health care or even typical systems are not responsive to this client group. Different things are possible.
Once in services, we need to prioritise the needs of the patient rather than the service or clinician. A lack of engagement might be the reason to work harder rather than to discharge. Seeking help in a way that alienates those who are supposed to care might be an issue to work on rather than a reason to shut the door. CMHTs are incredibly oversubscribed and under resourced so you could argue there isn’t the time. You could also argue that a year in a self-declared speciality hospital will cost you about six band-6 mental health professionals. Perhaps some of the high cost interventions could be avoided if we prepared our workforce better. Perhaps people who have typically been controlled will respond better to service models that emphasise choice. There is much more to look at, but useful things that we can be doing right now.

We need to prioritise patient needs – a lack of engagement might be the reason to work harder, rather than to discharge.
Statement of interests
Keir Harding and Hollie Berrigan have some influence in BIGSPDs decision to use Mental Elf services. They also both work for Beam Consultancy; “a unique organisation driven by clinicians and lived experience practitioners” who “provide training, consultancy and intervention for those living and working with complex mental health issues”.
Links
Primary paper
Ledden, S., Rains, L. S., Schlief, M., Barnett, P., Ching, B. C. F., Hallam, B., … & Johnson, S. (2022). Current state of the evidence on community treatments for people with complex emotional needs: a scoping review. BMC psychiatry, 22(1), 1-36.
Other references
Evans S, Sethi F, Dale O, Stanton C, Sedgwick R, Doran M et al (2017) Personality disorder service provision: a review of the recent literature. Mental Health Review Journal 22(2):65–82.
NICE (2009) Clinical Guidelines CG78: Borderline personality disorder: recognition and management.
Lamb N, Sibbald S & Stirzacker A (2018) “Shining lights in dark corners of people’s lives” The Consensus Statement for People with Complex Mental Health Difficulties who are diagnosed with a Personality Disorder.
Photo credits
- Photo by vahid kanani on Unsplash
- Photo by Priscilla Du Preez on Unsplash
- Photo by Lina Trochez on Unsplash
- https://stopsim.co.uk/
- Photo by Guillermo Latorre on Unsplash
- Photo by Miguel Orós on Unsplash
- Photo by Tim Marshall on Unsplash

Well said. I especially endorse your comments ‘Once in services, we need to prioritise the needs of the patient rather than the service or clinician. A lack of engagement might be the reason to work harder rather than to discharge. Seeking help in a way that alienates those who are supposed to care might be an issue to work on rather than a reason to shut the door.’ and ‘Perhaps people who have typically been controlled will respond better to service models that emphasise choice.’ which sadly
can apply as much to specialised in-patient hospitals as they may do to CMHTs.