
Welcome to the #EquallyWellAu23 live blog!
I’m Justin Chapman from Griffith University and I’ll be helping you keep up-to-date with all of the goings on at the Equally Well Australia National Symposium taking place in Sydney on 25-27th July 2023.
Experts from Australia and internationally are being invited to share innovative practice and developments aimed to improve the physical health and wellbeing of people living with mental illness.
I am a #BeyondTheRoom correspondent this week, working alongside Laura Hemming from The Mental Elf who is live tweeting this event. You can follow all of Laura’s tweets using the hashtag #EquallyWellAu23 or by following The Mental Elf on Twitter.
Page menu

Join us at the Equally Well 2023 Symposium in Sydney, Australia on 25-27 July 2023.
#EquallyWellAU23 live blog – promoting physical health in people living with severe mental ill-health
Like you all, I’m passionate about promoting mental and physical health, and this year’s symposium is looking to be a vibrant and productive event. We’ll be hearing from a range of national and international speakers presenting on developments in the policy, practice and research landscapes, and all focused on progressing toward the Equally Well vision of health equality for people living with mental health issues. Lived experience is central to policy, practice and research, and as always, lived experience underpins the values and themes of the symposium. I’m looking forward to engaging with lived experience perspectives, co-design and co-production, and the future of peer leadership in improving the health and wellbeing of people with mental health issues.
The first thing I noticed as I entered the symposium venue was the striking display of lived experience artwork collated from Out from the Mist, a global event for photographers, audio producers, and short film makers exploring lived experience through artistic mediums. I’ll be posting one of these images everyday and tagging the artists – these I feel have an interesting framing of hope, the process of recovery, and our relationship with the nature.

Out from the Mist submissions: A Caged Pigeon by Ryan Yangwentao; Untitled #1 to #4 by Lucy Brown; and Girl with the Sunflower by Zorica Purlija
You still have time to get your entries in, so get creative! The awards event will also be live streamed so check the Out from the Mist website for details.
Day one: 25th July 2023
We received a heart-warming Welcome to Country by Gadigal of the Eora nation elder Aunty Joan Bell. Aunty Joan told us about her younger years learning from the walk of life and her ancestors, and reflected on how a welcome to country is to establish an atmosphere of respect and honouring of the law of the country.
Emma McBride
The Assistant Minister for Mental Health and Suicide Prevention, Hon Emma McBride, then spoke about the importance of closing the gap in life expectancy for people with mental health issues, and particularly for First Nations people who experience a health gap irrespective of mental health issues. Emma spoke of laying the groundwork and setting an ambitious agenda to improve equity and access to care for people with mental health issues, and ensuring no-one falls through the gaps. The voices of people with lived/living experience of mental ill-health and suicide, and their carers, family and kin, are being elevated in the ongoing reform process. (Mental Elf tweet)
Catherine Lourey
It was a pleasure to hear from Catherine Lourey (NSW Mental Health Commission) who acknowledged that the Commission was established by the advocacy of the lived experience sector, and the voice of lived experience is key to the Commission’s role of improving health and wellbeing of the community. Emphasising collective action, Catherine said that harnessing partnerships with community and the Equally Well collective is key to driving reform for improved inclusion and health equality. The four cornerstones for success: (1) First Nations people who embody holistic and community centred approaches focusing on social and emotional wellbeing; (2) Evidence for guiding services within a socioeconomic context; (3) Partnerships for driving reform and enhancing change; (4) Collective action, embedding an ‘equally well’ ecosystem across government and non-government sectors to facilitate longer and more fulfilling lives for all people. Catherine highlighted that co-design and co-production are central processes for understanding and implementing solutions, as an iterative and ongoing effort. Catherine asked us all to reflect on two questions:
- How would you lead your life if you knew you had less time ahead of you, what would you change?
- In your role how can you break down obstacles to build an equally well country?
John Allan and Dave Peters
The highly regarded Co-Chairs of Equally Well, John Allan and Dave Peters, set the scene with their own welcome and acknowledgement of lived experience. Launching the next iconic policy document in the Equally Well series (following from the 2016 Consensus Statement and 2021 policy Roadmap) entitled Equally Well in Action (available in the Virtual Hub), John reflected on the 6-year journey since the Equally Well Consensus Statement was launched and achievements made to date, including 308 initiatives registered to improve the physical health of people with mental illnesses. Dave spoke of future directions, including (i) continuing the annual symposium and webinars for knowledge dissemination and professional networking, (ii) implementing physical health guidelines and expand Communities of Practice to build workforce capability, (iii) expand current initiatives, and (iv) improve evaluation and benchmarking through data linkage. (Mental Elf tweet)

Speakers at the Symposium opening: Catherine Lourey (top left), John Allan and Dave Peters (top right), John Allan (bottom right), Debbie Hamilton (bottom left)
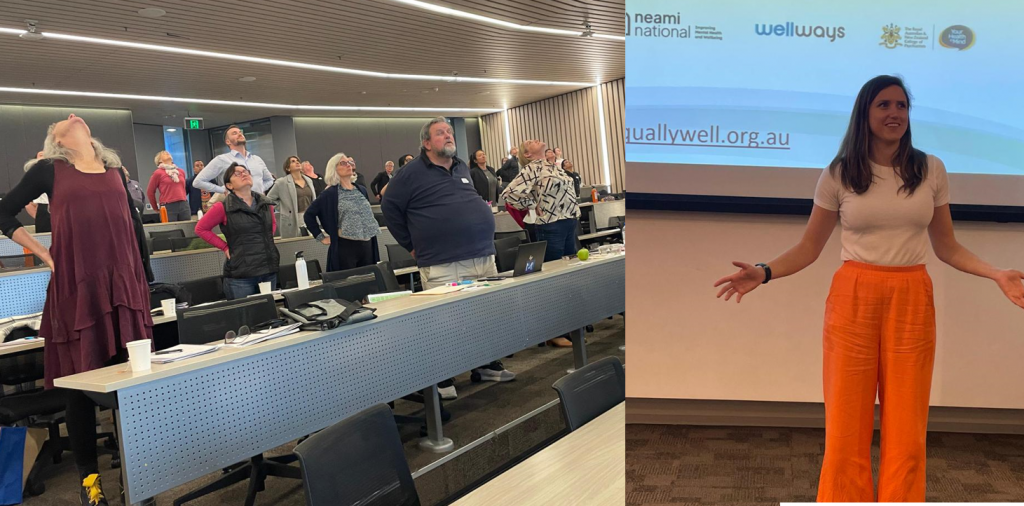
The flamboyant Andrew Watkins, Equally Well ambassador and co-developer of the Keeping the Body in Mind program, took the class for a yoga-based stretch session (Circle of Joy was my favourite).

Stretching break with Andrew Watkins (right) and the enthusiastic and engaged audience (left)
Debbie Hamilton
After our stretch break, we returned to a presentation by the eminent and charismatic Dr Debbie Hamilton, General Practitioner, Lived Experience Advocate, Equally Well Ambassador, and Board member of the highly influential national advocacy and research organisation Psychosis Australia. Debbie had an interesting start to the presentation by throwing us a curve ball – earmarked for talking about iatrogenic harm (harm caused by medical care), Debbie decided to talk about sex. A method of getting light-to-moderate (or vigorous) exercise and develop intimacy at the same time, sex has been pathologized and stigmatised. Talking about sexuality can be uncomfortable for people, but all people want to feel loved in their full humanity, and sexuality is one piece of that picture. The World Health Organisation states that sexuality is a central aspect of being human, and influenced by a broader biopsychosocial determinant framework. Historically, people with mental illnesses haven’t been seen as sexual beings like other people, and have been de-humanised in this aspect of their lives as well as other aspects. Very few healthcare workers ask consumers about sexuality and sexual side-effects of medications, however, nearly everyone with severe and persistent mental health conditions have had their sexuality impacted by medications. Social and cultural norms develop expectations of sexuality, which leads to exclusion and discrimination toward those who don’t ‘fit the mould’. Sexuality is a domain of quality of life, and healthcare workers need to consider the diversity and quality of life of consumers when developing and reviewing medication plans. The recovery model embodies the importance of social roles, and this includes the valued sexual roles in intimate relationships. (Mental Elf tweet)
Apparently Debbie’s presentation caused some heat because we were abruptly interrupted by a fire alarm…

An impromptu fire alarm interruption led us to an early lunch
Addressing inequities: symposium panel (11:25-12:25)
The panel discussion, “Addressing inequalities”, was Chaired by Catherine Lourey (introduced above) with esteemed panellists Dr Michelle Blanchard (University of Melbourne), Debbie Hamilton (introduced above) and Professor Richard Osborne (Swinburne University of Technology) and Harry Lovelock (Mental Health Australia).
Panel discussion with Harry Lovelock, Michelle Blanchard, Debbie Hamilton, and Richard Osborne, and Chaired by Catherine Lourey (left to right)
How do we address inequity?
Michelle: Three themes around dignity, respect and humanity are central to addressing inequity. Ensure that in all facets of a person’s life, people have an opportunity to choose a life of meaning and purpose. The experience of stigma and discrimination after accessing support from services is often the most damaging part of the experience.
Harry: Poverty is a policy choice that is allowed to exist because whether we admit it or not, there are people who benefit from exploiting the poor. Billions of government dollars inequitably support private sector services (including hospitals and schools), which is occurring alongside tax cuts for the wealthy and removal of tax concessions for low to middle income earners.
Debbie: “We can talk about rights as much as you like, but if you can’t afford a roof over your head, you can’t afford the $80 to go to a GP” (paraphrased).
Richard: Inequity is invisible – most people don’t see it because of inherent biases. Often if we do see it, it’s too painful and easily put out of our minds. We are blind to seeing the processes that we can implement now to impact the mechanisms of inequality and make a difference now.
What is that one area that could be tackled first?
Michelle: We treat things as a technical problem with a technical solution, but what we need to do is engage with complexity. There are interrelated factors that need to be addressed, and think about solving systems.
Harry: De-institutionalisation was based on changing the de-humanisation of people in institutional care. We do the same to people who are disadvantaged. We need reform in social support and taxation as a foundation to make gains toward improved equity.
Debbie: Newstart and pension allowance needs reform – how are people supposed to live on such a small amount of money so you can’t afford basic needs? People can be blind because they haven’t experienced what it’s like to be unable to make ends meet.
Richard: Many micro-solutions are needed, there’s no one-size-fits-all. People need to have basic securities met, such as food and housing. The challenge is competing agendas between health systems, policy, research and community members. When funding is spent in alignment with community values and needs, people have a better life.
What would your take-home message be?
Debbie: Government action should stem directly from conferences such as this where people say share their views.
Michelle: We all have responsibility in the decisions we make in our own lives. Engaging with lived experience to understand priorities, and take a scaled approach to addressing them.
Richard: “Care centred care” means deep engagement of all ‘actors’ involve in care. Let’s get gender equity right.
Harry: We’re facing a privatisation of healthcare. All the growth in mental health beds is in private hospitals, and NDIS is a privatised system. We need to understand that privatisation is not an effective system, and support block funding of services and universal health care.
Co-design and co-production (13:15 – 14:30)
As much as I wish I had Hermione Granger’s time turner device to capture all the great work of presenters at Equally Well, I was unfortunately limited to only one region of space-time… but the Mental Elf of Australasia Dr Laura Hemming covered the co-design and co-production streams of this event, and has posted key messages here: Mental Elf tweet.
I was fortunate enough to attend the ‘setting research priorities’ session…
Setting research priorities for physical health and mental illness (13:15-14:30)
Russell Roberts and Amanda Wheeler
The research priorities seminar was delivered by the National Director of Equally Well and Australia’s favourite man Professor Russell Roberts (Charles Sturt University) with Equally Well Ambassador, pharmacist extraordinaire and self-confessed Kiwi Professor Amanda Wheeler (Griffith University).
Amanda kicked us off with an overview of the research priority context. The Equally Well Consensus Statement has been the guiding document articulating research and implementation priorities in the physical/mental health space. Subsequent policy documents all similar things, focusing on integrating services, developing the workforce, embedding lived experience into usual practice, driving quality improvement, data integration, and dedicated funding for this important area. We’ve had small, targeted pockets of funding, but very little at the national level: the National Health and Medical Research Council had two targeted calls for translational research; however, one scheme was allocated for a single national network, and the other had a total value of $5 million for research nationally. There are significant funding gaps to address these concerns.
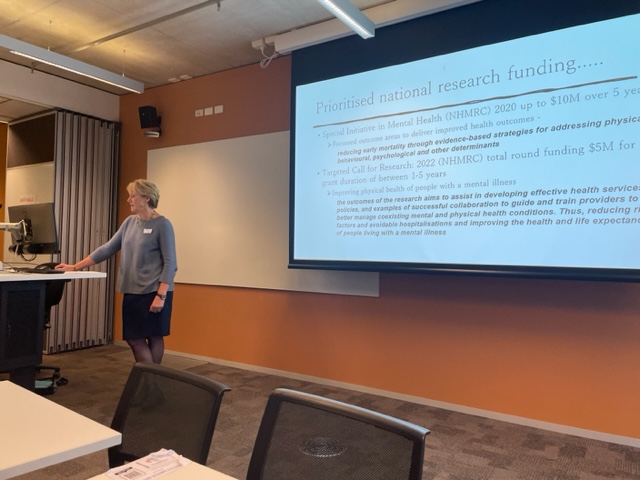
Prof Amanda Wheeler presenting on the policy context of priorities for research and implementation to achieve the vision of Equally Well
To engage the audience for mapping gaps in translational research, Russel presented preliminary results of Equally Well’s research scoping survey. It appeared that work in alcohol and other drugs (AOD) over the last 12 months is under-developed. Equally Well has initially focused on mental health, and Russell hinted that there might be a change in the future to expand more into supporting AOD services. The audience noted that peer work wasn’t picked up on the scan at all. When asking about specific health conditions, most research is about general health and wellbeing. Predominant methods included qualitative methods, survey methods and co-design projects. Most projects were with general adult samples, with a lack of projects with people from culturally and linguistically diverse backgrounds.
Russell and Amanda facilitated brainstorming sessions about how we could secure more funding specific to improving the physical health of people with mental illness. People spoke of cross-agency collaboration, supporting research capability, monitoring, evaluation and reporting, public communication to improve awareness and advocacy with a coherent message, working with philanthropy and health insurance companies to build investment and demonstrate return.

Brainstorming session with the audience, facilitated by Amanda Wheeler and Russell Roberts
Partnerships (15:00-16:25)
Sally Plever and Irene McCarthy
Next, I was privileged to attend the Partnerships stream Chaired by Dave Peters (introduced previously). First in the line-up were the leaders in state-wide reform to improve the focus on physical health in Queensland public mental health services Sally Plever & Irene McCarthy, who lead the QLD Mental Health Clinical Collaborative (MHCC). Sally and Irene have been the guiding light for smoking cessation and systems change over the past 7 years in our maroon jersey wearing state (if you like football, which I don’t). They were accompanied in spirit by MHCC Chair, the prolific and charismatic Professor Dan Siskind, a visionary of physical/mental health research in QLD Health and an accomplished yoga practitioner – you’ll be getting some expert instruction from Dan later this afternoon.
Sally and Irene from the QLD Mental Health Clinical Collaborative giving an Acknowledgement of Country
Sally and Irene launched a state-wide mapping resource developed in collaboration with the Diabetes Clinical Network entitled Supporting metabolic health for Queenslanders living with serious mental illness &/or substance use. This document was developed by a large network of QLD Health staff including clinicians, academics and people with lived experience. The working group identified all initiatives in QLD Health that addressed the physical health of consumers, and each initiative was mapped for the lifestyle factor it addressed, the consumer group that the programs are for, and what’s involved with delivering the program. Most programs lacked evaluation; however, all programs included highly motivated and hard-working clinicians working in multidisciplinary teams to improve outcomes for consumers. Sally also highlighted the outstanding achievements led by the MHCC in reducing smoking rates in Queensland.

Queensland Health document developed by the Mental Health Clinical Collaborative (MHCC) in partnership with the state-wide Diabetes Clinical Network
Amanda Wheeler and Victoria Stewart
Next we heard from Prof Amanda Wheeler (introduced previously) and Occupational Therapist extraordinaire Victoria Stewart (Griffith University) who presented some of the great outcomes of PharMIbridge, their national cluster randomised trial to with community pharmacies. You can read the protocol for this study here, and their training program for community pharmacists here.

Vicky Stewart (left) and Prof Amanda Wheeler (right) presenting on community the pharmacist’s role in goal setting with people with mental illness to support improvements in wellbeing and lifestyle change
I’ve always thought of pharmacists as the people who help me get Codral with pseudo in it when I’m sick, but this innovative study is pushing the pharmacist’s scope to have a more person-centred role. Community pharmacists recruited from Queensland, Western Australia, and New South Wales who participated in a one-day training program to improve communication, confidence, goal setting and motivational interviewing to support people with severed and persistent mental illnesses with their medications and to improve health and wellbeing.
Vicky’s recently published taxonomy for goal setting between people with mental illness and pharmacists is available here. Consumers felt they could trust their pharmacists with these discussions and had improved satisfaction with medications and experiences with the community pharmacy, and the pharmacists enjoyed connecting with consumers to support their wellbeing.
Carmello D’Aquillino and Lachlan Best
Dr Carmello D’Aquillino and Occupational Therapist Lachlan Best gave us some great insights into the challenges and enablers of integrating healthy lifestyle support into routine clinical care in Older People’s Mental Health Services at the South Western Sydney Local Health District.
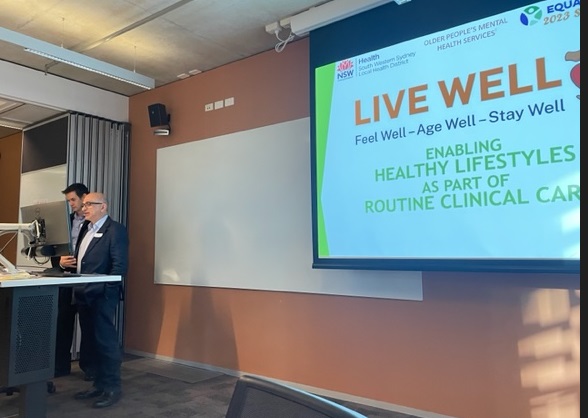
Lachlan Best (left) and Dr Carmello D’Aquillino (right) presenting on their Live Well program
Healthy lifestyle change and behaviour modification is an art – both in terms of helping someone to change their lifestyle behaviour, as well as supporting staff to change their practice to include lifestyle support in usual care. The Live Well program is founded on the transtheoretical model to explore lifestyle behaviours with consumers, and leverage the therapeutic relationship to enable self-directed positive action. Evaluation of the program indicated that consumers were highly satisfied with the program, and had improved wellbeing after 12 weeks. You can see their video overview here. The program includes a clinician toolkit and local resource guide to support community integration, and the team have also translated the resources into six languages.
Debbie Beahan and Mitchell Goodwin
This session was concluded by Debbie Beahan and Mitchell Goodwin who gave an insightful account of the challenges involved with integrating care across Western NSW for First Nations people. The presentation was cleverly named “Keeping the mob in mind”, to remind us all that the health disparity faced by Aboriginal and Torres Strait Islander people is largely caused by socioeconomic challenges faced by their communities, that need to be addressed as a human rights issue (and perhaps as a hat-tip to the Keeping the Body in Mind achievements).

Debbie Beahan and Mitchell Goodwin presenting their work and impact of implementing comprehensive support service models for First Nations people
They presented on Planned Care for Better Health and Emergency Department to Community, which embodies a culturally responsive person centred, comprehensive and coordinated approach to care for First Nations people presenting with chronic health conditions and complex social care issues at risk of hospitalisation. It’s delivered a team of multidisciplinary care coordinators working across hospital, primary care and community settings. Mitchell took us through a case study example of incremental progress with someone sleeping rough, getting small wins that lead to big wins and better connection with family and kin. The holistic nature of this innovation is depicted nicely in the below slide about powerful partnerships.

Partnerships are powerful: Slide image from Mitchel and Debbie
Day 1 – closing presentation: Richard Osborne
Professor Richard Osborne (introduced earlier) wrapped up the day with a cracking presentation about health literacy and reproducibility in research. Most of the research we do is not reproducible – the indicators that drive research, such as publication output and citations, is what drives research so reproducibility is undervalued. Reproducibility matters because it improves the usefulness of programs. A top-down approach for program design is when governance is distal from communities, and improvements are based on prior evidence. The bottom-up approach can be transformational through community activism and mobilisation of resources, but participation can be fragmented and disconnected from policy processes. Policy and programs need to be matched to what the community needs and can be implemented, which improves reproducibility and supports scalability of health literacy interventions.
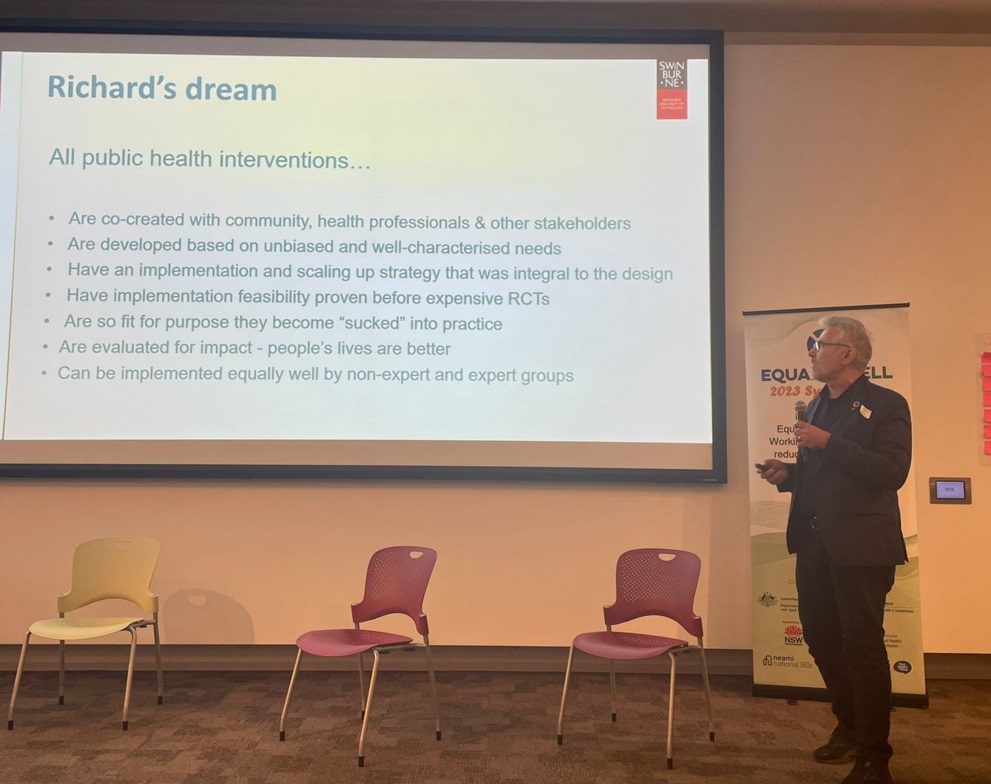
Professor Richard Osborne presenting his dream of public health interventions, and remarkable progress that he and his teams have made in this area
The health literacy dilemma is that people’s beliefs and attitudes and beliefs are not necessarily aligned with public health advice on disease prevention. Health literacy can be considered at three different levels: (i) individual, (ii) community and (iii) health literacy responsiveness. Health literacy is a social practice, where our decisions are highly influence by social and cultural norms. A well-considered mix of interventions is needed for disease prevention, and a variety of media is needed in effective messaging.
Richard presented data on responses to the Health Literacy Questionnaire, and demonstrated clusters of people with similar scores indicating different strengths and methods of engaging with health information. Their NSW Health Literacy Initiative resulted in resources to help health workers’ understanding about mental health. The Ophelia framework for health literacy interventions emphasises changes in organisations, staff, individuals and community engagement to reach as broad a community audience as possible Action areas to build system-wide responsiveness included (i) connection between health services and communities, and (ii) accessing help at the right time in easy friendly ways.
Wrap up: Dan Siskind
We missed our scheduled stretching break this afternoon, but as promised, Professor Siskind has kindly offered some stretching and mindfulness advice from afar. If you’re following along at home, Professor Siskind says stand firm in Warrior pose with spine erect, breathe into your abdomen for the count of 10, then repeat on the other side.

Professor Siskind takes us for a stretching session in spirit. Note: Dan’s express consent was obtained to misappropriate his image.
It was an eventful day, and there was no better way to finish it off then some networking drinks sponsored by Queensland Health.
Day two: 26th July 2023
For the virtuous early birds, today began with a social walk at 6:30am – I genuinely hope you all enjoyed the sunshine and fresh air. Those who networked a little too hard last night may have enjoyed a couple of hours extra sleep, and we opened promptly at somewhere between 9 and 9:30am.

A cross-section (admittedly somewhat Queensland-biased) of well-meaning and enthusiastic attendees of the Equally Well networking event, sponsored via a transparent and impartial process.
As a diligent individual I attended early to get the front seat. Whilst sipping my latte and enjoying the Out from the Mist display, I was struck by the poignant displays of lived experience artwork. Here are some more exhibitions from people across the globe who are exploring possibilities using artistic mediums.
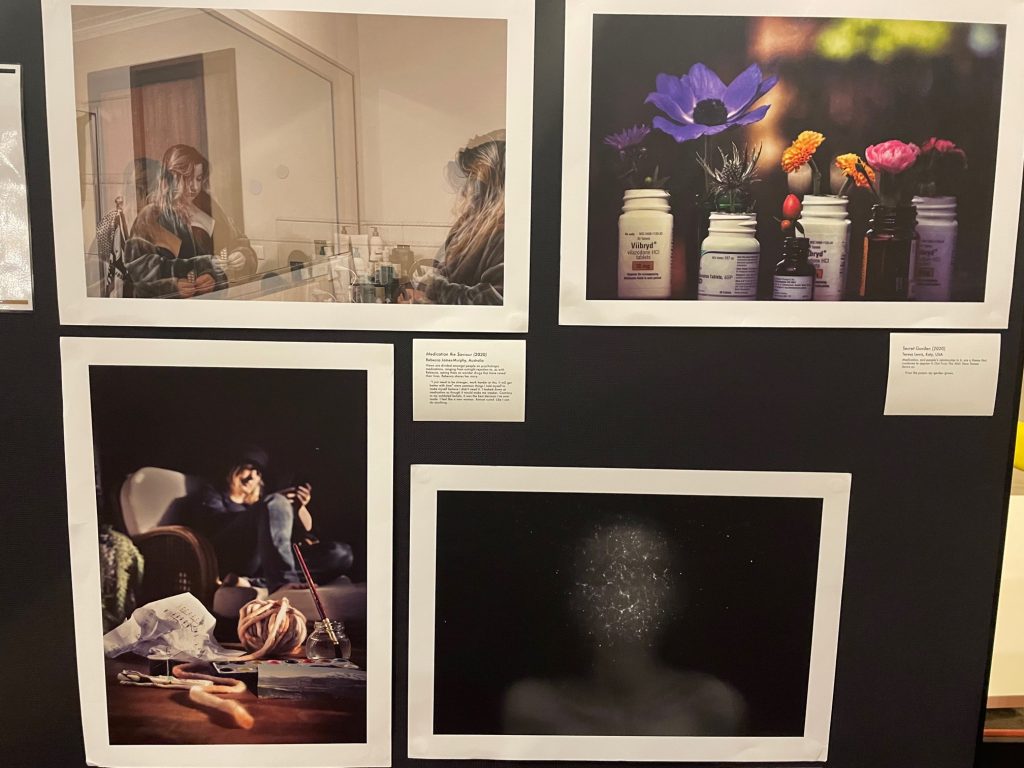
Medication the Saviour (top left) by Rebecca James-Murphy; Secret Garden (top right) by Teresa Lewis; Night Echoes (bottom right) by Emily Jansell, and Hypomanic/Procrastinate, and Repeat (bottom left) by Catherine George
Opening
We were once again greeted by our fearless leaders Dave Peters and John Allan. Dave opened Day 2 of the Symposium respectfully, acknowledging the Traditional Owners of the lands upon which we’re all meeting.

Dave Peters welcoming us to Day 2 of the event
After an acknowledgement of lived experience, Dave handed over to Rose Jackson (NSW Minister for Mental Health) to provide a unique welcome.
Rose Jackson
Rose said that when it comes to making change, research and facts are important, but the key ingredient is people telling their stories. People who are brave enough to tell their truth forms the powerful change agent we need. We know the statistics – people with mental illnesses die younger and are more likely to be hospitalised for physical health reasons than the general population – that’s why taking the time to engage in this conversation is important. We can’t achieve our goals without a partnership between government and the research and lived experience community, and today’s launch of the Keeping the Body in Mind(gardens) Digital Physical Health Resources will provide a clear Roadmap developed in partnership between the NSW Mental Health Commission and Prof Jackie Curtis from Mindgardens. The link between housing and mental health is essential, but the picture is broader, and the issues facing people with mental health issues need to be elevated in government priorities. Even in health settings the link between mental and physical needs to be acknowledged more deeply. People with mental illness have every right to access the same level of care as everyone else, and the biggest gaps we need to close are in mental health settings.

Rose Jackson (NSW Minister for Housing, Minister for Homelessness, Minister for Mental Health, Minister for Youth)
Jackie Curtis
This was followed up by a Special Event delivered by a celebrity in the physical/mental health world who needs no introduction, Professor Jackie Curtis, Executive Director of the Mindgardens Neuroscience Network. Jackie led development of the Early Intervention Framework which has been adapted for use in nine different countries (the most recent UK update available here), and spearheaded a suite of Keeping the Body in Mind programs tailored to primary care, vaccines, smoking cessation, and culturally and linguistically diverse groups along with her team and collaborators.

Professor Jackie Curtis launching the KBIM Resource package, culmination of a 20+ year journey of research and implementation
The evolution of these programs and resources is shown below over a 20+ year timeline. In partnership with NeuRA, Black Dog Institute, University of NSW, and South Eastern Sydney Local Health District, they have influenced systems change at multiple levels to impact translational research, education and training, policy and consumer co-production. The resources were co-designed between people with lived experience and a committee of international multidisciplinary experts, and includes three clinical frameworks for positive cardiometabolic health, and 17 modules for goal setting to support healthy lifestyle changes. This is a body of work and resources to add to the collective impact of the Equally Well ecosystem.
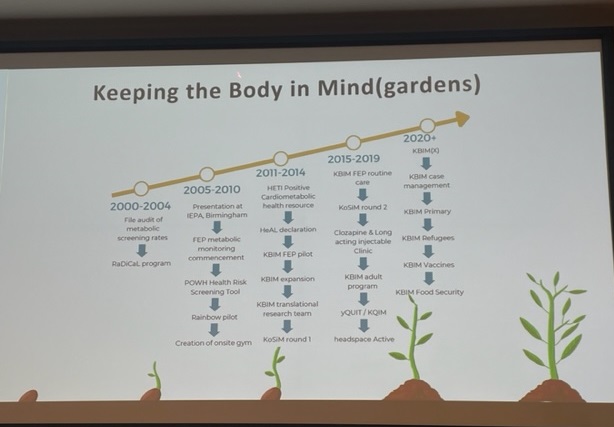
The history of Keeping the Body in Mind(gardens)
Break
We all love stretching here, and this time we were led by Law who took us through some delightful stretches to reinvigorate us for the day (my favourite was the Standing Cat-Cow)…

Law taking the class for some relaxing body opening
Felice Jacka and Tetyana Rocks
Professor Felice Jacka and Dr Tetyana Rocks from the Food and Mood Centre need no introduction for anyone who follows the literature on nutrition and mental health. Professor Jacka has been credited with developing the field of nutritional psychiatry (yeah, she developed an entire field of research, what have you done lately?), which has impacted global policy and international clinical guidelines. Tetyana focuses on translation, with the development of innovative educational courses and implementation with mental health services.

Professor Felice Jacka (left) and Dr Tetyana Rocks (right) presenting on nutritional psychiatry and the SMILES trial
Felice spoke about how there is a very clear link between diet quality and common mental illnesses such as depression and anxiety. The problem is that all the focus has been body size and weight; however, the evidence indicates that a stronger focus on brain health can more effectively prompt behaviour change. People who have a healthier diet are 30-35% less likely to develop depression, independent of socioeconomic status, other health behaivours (e.g. physical activity, smoking etc), and it’s not explained by body weight. The quality of diet is linked in a dose response relationship with mental health. We see this relationship across the world, and across the life course, from the intrauterine environment and diet of the mother, to early development and adolescence, adulthood and into the older years. The Royal Australian and New Zealand College of Psychiatrists (RANZCP) practice guidelines include lifestyle factors as a key treatment for mood disorders, and it’s a highly cost-effective treatment. The SMILES trial was the first to investigate the Mediterranean diet for people with diagnosed depression, which demonstrated a 32% remission of depression in people who received the dietary group compared with 8% remission for people who received social support.

The SMILES diet, and some tips for helping people make healthy eating changes
Tetyana then took us through the Mediterranean style diet that was used in the SMILES trial, which was adapted to combine with the Australia Guidelines for Healthy Eating. The diet has a high consumption of nutritious and wholesome foods, such as fruit and vegetables, healthy fats and whole grains. Dietary interventions led by accredited professionals are more effective because of their knowledge and way of engaging people with food, and the SMILES trial was delivered by dietitians. Helping people to improve their diet (or change any kind of behaviour) is an art, and requires good timing, attention, acknowledging small successes, encouragement, barrier breakdown, and ongoing follow-up. If you’d like to learn more about implementing nutritional psychiatry in practice, you can access their courses here.
Where to next? (Panel discussion 10:45-11:45)
This panel was Chaired by Australia’s favourite man Prof Russell Roberts (introduced yesterday using the same tag line) – see below for a collage of Russell, beloved by all.
Professor Russell Roberts (top left, top right, bottom left, bottom right)
The discussion focused on the future of turning policy into practice. Panellists were Dr Ruth Vine (National Mental Health Commission), Tricia O’Riordan (NSW Health), Cat Goodwin (Central Eastern Sydney Primary Health Network), and Carolynne White (MIND Australia).
Insights for how to convert policy to practice
Carolynne: We need to consider the ‘who’, ‘what’, ‘how’, ‘when’ and ‘where’: (i) who was involved in co-designing the policy and who’s voices were heard or missing; (i) what are we trying to change, making a real change in physical health comes to address the social determinants; (iii) how we do it needs to incorporate lived experience and practitioner wisdom (iv) when do we introduce these conversions, trust and rapport is needed, and people have many competing priorities; (v) where we should start is wherever we can touch – do what you can, where you can, when you can.
Tricia: Listening is invaluable – it’s not enough to just acknowledge it, we need to act on it. We need to make sure that everything in policy is informed by the people we’re serving. We need to be honest and upfront about what’s being asked, the possibilities and limitations, and keep people informed along the way. Partnerships are pivotal, and we need to use the power of partnerships to make change for maximum benefit. One size won’t fit all, so policies need to be adaptable and flexible.
Ruth: Key things that can enable or block progress are resources, people and systems. In order for things to work we need ongoing resources, relationships and systems. There is an overarching equity policy; however, we know from our evaluations of Better Access that in reality there are different outcomes for different people. Changing Medicare billing items to better address people who are disadvantaged can help to address this gap sustainably. Sustainable and scalable/generalisable improvements to the system isn’t possible with strong leadership.
Cat: One of the main levers for Primary Health Networks (PHNs) are the commissioning practices and processes. PHNs can commission programs that adhere to the latest guidelines and incorporate co-design, and prioritise integrated models of care. There is opportunity for PHNs to amplify their impact through outcome measurement, service delivery outputs, consumer rated measures of service provided, which could shift practice in the tight direction. PHNs are funded for local solutions, but there is scope for working together across regions to support scalability.

Panel discussion on policy to practice. From left to right: Cat Goodwin, Ruth Vine, Tricia O’Riordan, Carolynne White, Russell Roberts.
What are some of the ‘landmines’ or ‘pitfalls’?
Tricia: We can write the best policy, but if there aren’t implementation partners in the ‘real world’ it won’t go anywhere. There needs flexibility in partnership rather than demanding action.
Ruth: Know who you’re engaging with before you take the steps. If you don’t have your engagement correct when you’re dealing with a workforce under pressure, you’ll meet a lot of barriers.
Cat: When things go wrong it’s often when it’s rushed, but with good partnerships solutions can be found.
Carolynne: If you don’t challenge your own biases and consult people who know the topic, you can go down the wrong path. Also, it doesn’t stop with co-design – time needs to be allocated for fully implementing the product.
Questions and reflections
The panellists then reflected on their successes, but acknowledged that it’s difficult to achieve outcomes that are sustained. Often the outcomes aren’t seen immediately, and investment now can lead to unanticipated rewards down the track.
A question about resourcing and support for embedding evaluation into usual practice was raised. Building research capability and embedding an ‘evaluation culture’ in mental health workforces is a priority articulated strongly in the Productivity Inquiry into Mental Health recommendations. Mentoring and training for clinicians is needed, and Communities of Practice need to be supported. Mindgardens has developed MindLabs to support quality improvement, and Jackie Curtis provided an open invitation to all to reach out for support.
An audience member raised the issue of medication insecurity as a component of wellbeing. Ruth Vine noted that there are many issues related to supply of medication, so it needs to be address at multiple levels. If you’re interested in this topic, tune in for a panel discussion this afternoon about medications.
Take-home messages
Cat: People are really happy to share their expertise – ask for help.
Ruth: Be mindful of the area in which you work and be opportunistic, allying your self with supporters.
Tricia: Don’t let ‘perfect’ be the enemy of ‘good’
Carolynne: Reach out for lived experience expertise and practitioner-based wisdom.
Simon Rosenbaum
The room filled with delight as global citizen Associate Professor Simon Rosenbaum spoke about international work that he was leading, contributing to, and being a part of, all geared toward improving capability and capacity of mental health workforces to address emerging community needs. Nicknamed on social media as “The Baum”, Simon is widely regarded as the poster boy of physical activity for mental health, and has worked in low-middle income countries to support mental health workforce development in many ways, including through sport and physical activity.

Associate Professor Simon Rosenbaum
Simon started with a quiz for self-rating your physical health competency if you’re a mental health professional, then provided some take-away messages in song form: (1) I get by with a little help from my friends (The Beatles), indicating social support and resources to match needs; (2) I can see clearly now the rain is gone (Johnny Nash), indicating new beginnings for mental health workforces; (3) If you fall I will catch you, I will be waiting (Cyndi Lauper), relating lifestyle programs to a safety net for accessing support and promoting engagement with people who are disadvantaged and at risk; (4) Now I’m freeeee, free fallin (Tom petty), funnel into traditional mental health services; (5) We are family (Sister Slege), co-production and co-delivery essential.
Simon related the Mental Health and Psychosocial Support Pyramid to providing physical activity intervention. First, a basic level of infrastructure is needed, but it doesn’t stop at just havingthe equipment. Secondly, community sport and activity programs need to be delivered. Thirdly, general mental health awareness and training for facilitators is needed to improve acceptability of programs. Finally, if possible, tertiary qualified exercise professionals are needed to maximise the benefit of programs.
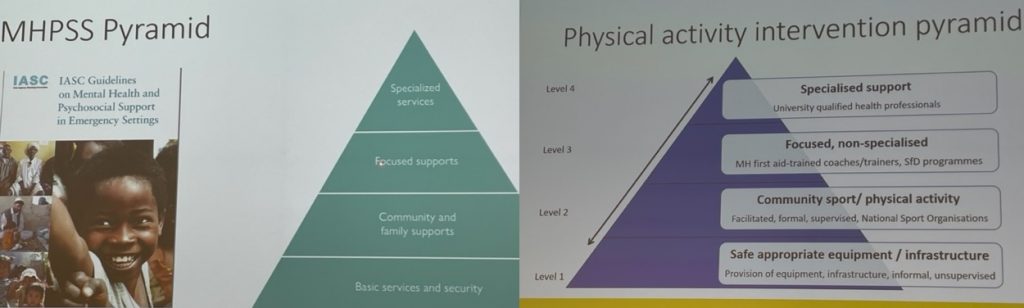
The physical activity intervention pyramid, adapted from the Mental Health and Psychosocial Support pyramid
Addi Moves is a real-world example of a program to improve food security and physical activity of people from culturally and linguistically diverse backgrounds, which is situated nearby other health and social services to improve integration. The co-design outcomes of how this space was developed is currently under review (lead author Grace McKeon); key messages from participants included the necessity for cultural safety, accessibility, physical activity literacy, social connection, and ensuring basic needs are met.
Chris Maylea
After lunch we were treated to another Special Event. Associate Professor Chris Maylea brings a mean combination of social work and law to the table, which is just the balance needed to bring human rights and social justice to the forefront of conversation. Underpinned by co-design approaches, Healthtalk elevates the voice of lived experience in generating resources for improving the physical health of consumers.

Associate Professor Chris Maylea launching the resource Healthtalk
Chris and his team did a review and found that the consumer voice is often neglected in physical health research (here). To develop the resource, they spoke to 32 in Victoria and NSW with the support of Neami National, who reported having experiences with a variety of physical health conditions ranging from sleep apnoea and joint pain to cancer and heart disease. Chris mentioned a randomised controlled trial (NEON-O), demonstrating that providing access to recovery-oriented narratives improves outcomes for people with mental illness, but may not be as effective for people experiencing psychosis.
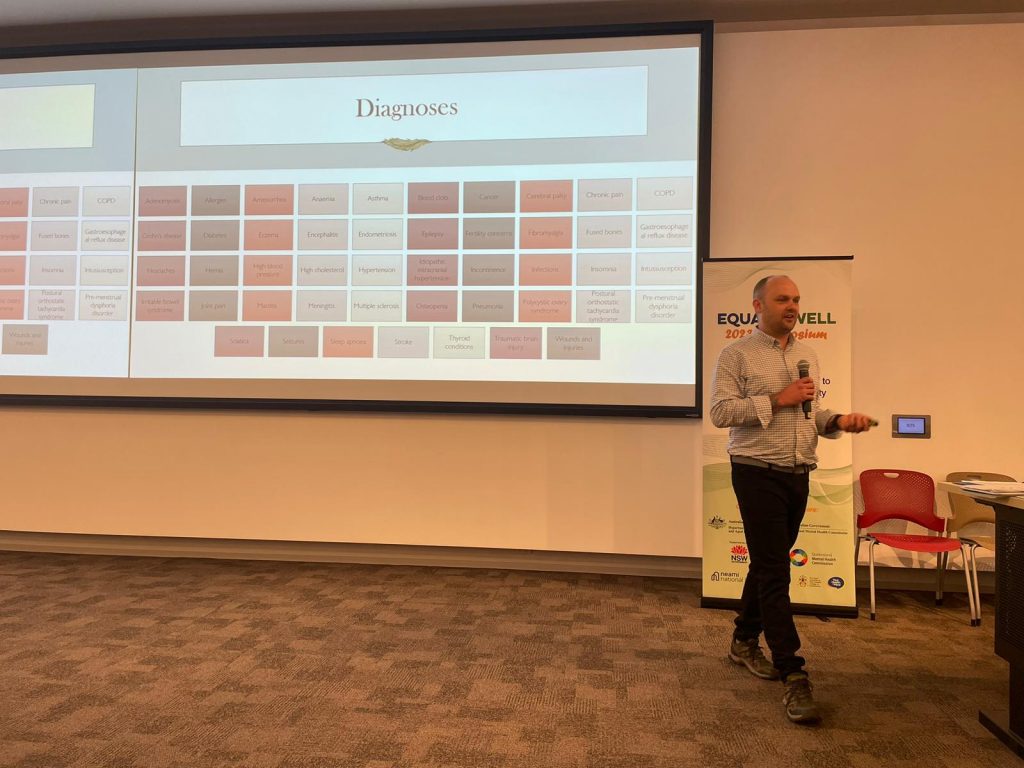
Chris presenting on the variety of physical health experiences reported by people with lived experience who contributed to Healthtalk
In the findings from Chris’s investigation, one of key factors in people’s recovery was the therapeutic relationship with mental health workers, and the simple actions and compassionate gestures made all the difference to the experience of mental health support. People reported that it was a tough journey, and they needed to self-advocate which can be extremely difficult to do while experiencing other life challenges. Healthtalk provides people with exposure to other people’s experiences, which can be very validating and help them develop a broader understanding of their experiences.
Matt Tindall
Following this we heard from Matt Tindall (Aboriginal Mental Health Director, NSW Health) who presented on Cultural determinants of Aboriginal Mental Health and Wellbeing. Matt was originally from Narrabri country in North West NSW, and brings his experiences into his practice to elevate lived experience within mental health and suicide prevention. After a respectful Acknowledgement of Country, Matt presented about the cultural determinants of health.

Matt Tindall providing Acknowledgement of Country
Matt’s vision statement was that “Aboriginal health is everyone’s business”. There are over 300 different clan groups or ‘nations’ across Australia, so there’s no one-size-fits-all approach. Improving the health of First Nations people needs to be considered in a historical context, because it’s directly related to current day lived experiences of community members. The 5-year Aboriginal Mental Health and Wellbeing Strategy articulates goals for improving (i) holistic and family centred care, (ii) culturally safe and trauma informed care and (iii) connected care.
As well as supporting communities to be Equally Well, we need to support them to be culturally well. Cultural Wellness involves connection to country, cultural beliefs and knowledge, self-determination and autonomy, family and kinship, cultural expression and continuity, and leadership in decision-making. Traditional medicines are integral to health for Indigenous Australians; however, traditional healers aren’t recognised in Australia. The 2013 Hand-on-Hand report highlighted the under-recognition of the 60,000 year-old Aboriginal medical knowledge system.

Matt Tindall providing advice and recommendations for the future direction of better mental healthcare for First Nations people
Matt spoke about culture-bound syndrome experienced by First Nations people, such as longing for country, sorry cutting, sorry time, being sung/payback, and spiritual visits, which can be misinterpreted as symptoms of mental illnesses. Cultural competency needs to be integral to systems and services, and traditional healers and medicines need to be incorporated in health systems, similar to how other cultural medical approaches are recognised in Australia (e.g. Chinese medicine).
Break
This afternoon’s stretching break was led by an accredited exercise physiologist (AEP) from Keeping the Body in Mind program… sorry, I missed her name…
KBIM exercise physiologist leading the afternoon’s stretching session
Panel discussion: Medications and managing side-effects
The only thing we love more than stretching here at Equally Well Symposiums is panel discussions. Particularly if we get to hear from movers-and-shakers such as Prof Amanda Wheeler (introduced quite a few times now), Vicki Langan (Neami National), Lauren O’Donoghue (Neami National), and Rod McKay (HETI, NSW Health). Our Chair for this panel was Associate Professor Caroline Johnson (University of Melbourne).

Panel discussion on medication side-effects: Lauen O’Donoghue, Vicki Langan, Amanda Wheeler, Rob McKay, Caroline Johnson (left to right)
Lauren: (1) Importance needs to be paid to co-morbidities and taking in the bigger picture. There are dire consequences for prescribing medications to people without considering the whole person. Prescribers who make quick judgements when prescribing put people’s welfare at great risk. (2) Communicate and collaborate with consumers and the wider care team. Side-effects need to be explained, otherwise people can become very distressed by the impact of side-effects. (3) Person-centred approaches are essential, remembering that the person is the expert of themselves – listen to what they say and feel. Ask them about their experiences rather than presuming and inferring.
Vicki: Neami developed guidelines for staff and consumers about having a conversation about medication. Many staff don’t see it as their role to have that conversation, so Neami co-designed guidelines to frame the conversation to improve confidence. Consumers want support workers to advocate for them; however, commonly both consumers and staff feel disempowered in that conversation with clinicians. One of the emergent recommendations was supporting a conversation around ‘area of concordance’ where the consumers and clinician come to an agreement for their medication plan.
Amanda: (1) Shared decision making, aligned with Vicki’s point about concordance and Lauren’s point about listening. Medication plans need to be very individualised, and involve ongoing monitoring. (2) Communication is needed to mitigate medication related problems and harm, with the consumer and their family, and the wider care team. (3) Medication review to monitor side-effects, treatment burden, effectiveness; utilising services such as Meds Check and Home Medicine Review, accessible by referral.
Rod: Using medications well is a team endeavour. Important not to ‘set and forget’, things can change over time and regular review is needed. Prompts and postcards can help to enable the conversation. We can’t forget that despite their problems, medications have many benefits, and result improve quality of life and improved life expectancy.
What would be most useful
Lauren: It’s always good to have visual aides and resources so consumers can walk out with the information. Clear expectations and accountability about ensuring that consumers have the full story.
Vicki: Asking them how much information they want to know. Sense of caring and connectedness between the prescriber and the person their treating is needed.
Amanda: Seeing where the person is and how much information they want to take on. Much of our current research is about getting GPs and community pharmacists to work together more closely in regional areas to improve communication.
Rod: There’s usually a short list of things that people would like to know, or need to know. An important discussion is reducing the medication, and often people don’t want to reduce medication because the side-effects can sometimes outweigh the risks.
An audience member suggested this resource for regaining power during medication appointments by Pat Deegen.
The inaugural Equally Well awards
The event we’ve all been waiting for is the Inaugural Equally Well Awards. Whatever came before this was warming-up the audience for these headlining acts, and we were all looking forward in anticipation to celebrate those contributors who have made an impact to achieving the Equally Well vision of equality of life for people with mental health issues. John Allan and Dave Peters led the award presentations.
Outstanding individual contribution was awarded to Professor Rosemary Calder (Mitchell Institute, Victoria University). Highlights include publication and dissemination of the Being Equally Well Roadmap and advocacy for increased funding in the sector.

Rosemary Calder accepting the Outstanding individual contribution award
Outstanding team effort was accepted by Professor Jackie Curtis (Mindgardens Neuroscience Network) on behalf of the Mindgarden Neuroscience Network team: Jackie Curtis, Hamish Fibbins, Patrick Gould, Oscar Lederman, Rachel Morell, Catherine O’Donnell, Simon Rosenbaum, Scott Teasdale, Phil Ward, Andrew Watkins.

Jackie Curtis accepting the Outstanding team effort award on behalf of the KBIM team
Outstanding co-design was accepted by Vicki Langan on behalf of the Neami National team: Vicki Langan and Whitney Lee. Their co-designed Indigenous Health Prompt is a result of the need to increase accessibility and improve health literacy of Indigenous consumers.

Vicki Langan accepting the Outstanding co-design award
Emerging Star Award was awarded to Suhailah Ali (University of Queensland) for her PhD work in Understanding the contribution of psychosis and bipolar disorder to premature mortality.

Suhailah Ali accepting the Emerging Star Award
Research Impact Award was accepted by Dr Grant Sara on behalf of the team: Grant Sara, Jennifer Humphrey, Fred Wu, Wendy Chen, Patrick Gould. Mental Health Living Longer (MHLL) is a translational research project supporting efforts to reduce premature mortality in NSW mental health service users.

Grant Sara accepting the Research Impact Award on behalf of the team
Outstanding Partnership & Collaboration Award was accepted by Christine Kaine on behalf of the team: Christine Kaine, De Backman-Hoyle, Simon Stafrace, Eileen Lavranos, Bronte Jeffries, Simon Byrne, Sharon Lawn and the RANZCP Policy & Engagement Team. In 2019, the Royal Australian and New Zealand College of Psychiatrists Community Collaboration Committee (CCC) identified loneliness as a neglected factor in the understanding and care of mental illness. The CCC surveyed over 300 consumers to develop resources and recommendations.

Christine Kaine accepting the Outstanding Partnership & Collaboration award on behalf of the team
Outstanding Service Award was awarded to Professor Russell Roberts for all his leadership and advocacy to improve outcomes and equality for people with mental health issues, nationally and internationally. In true Australian style Russell referenced how good we are relative to our population size, “The work we are all leading is really world class, and per capita we are leading the world in this area”. I told you he was Australia’s favourite man!

Russell Roberts accepting the Outstanding Service Award

All award winners
Closing presentations
Chris White
Following this, we heard from Chris White (Mental Health Foundation, UK) who presented online, and who spoke insightfully in his presentation aptly named “No health without mental health, No recovery without physical health. Addressing the health inequalities elephant in the room”. Drawing on wisdom from over 20 years of incorporating his own experiences into elevating lived experience leadership across mental health sector, Chris have an account of how his experiences have informed his work in the physical/mental health space.
Chris White speaker of his experiences with recovery, and how mental and physical health are interrelated.
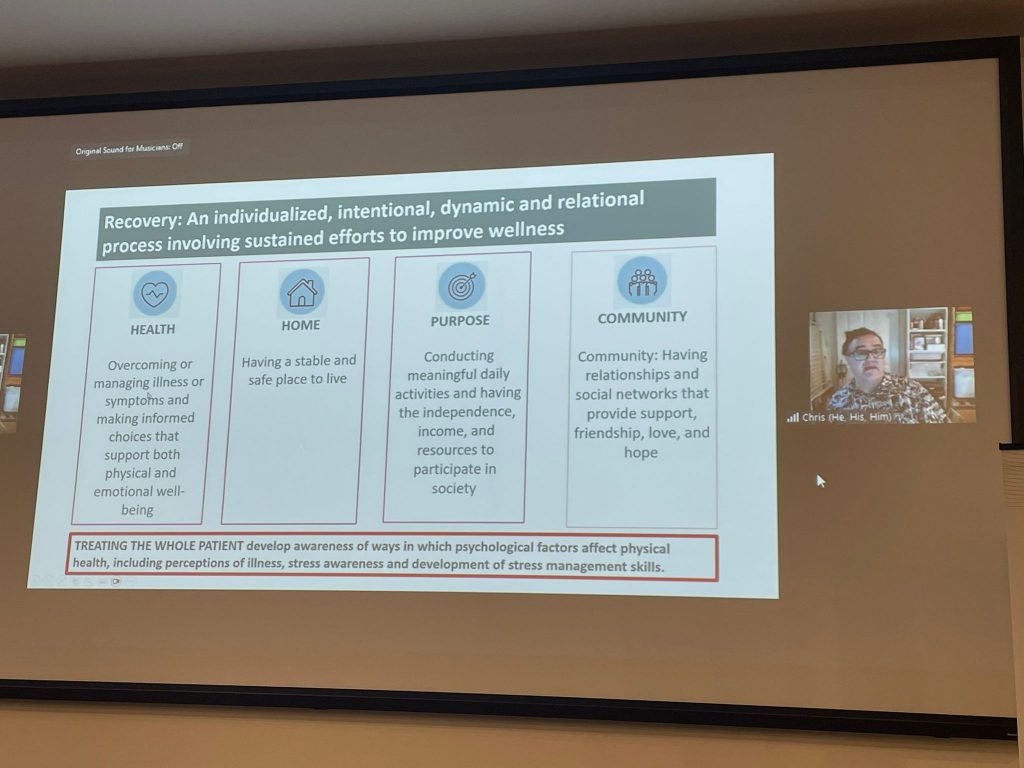
Chris referred to the first time that modern medicine began recognising the link between physical and mental health. We now know that people with mental illness have significantly higher risk of preventable physical disease than the general population. Chris reflected on his own recovery journey involving smoking and alcohol consumption that was not address in mental health service, which led to physical health complications and significant surgery. Recovery is not just about mental health recovery, it’s a whole-of-person and whole-of-life approach. We need to start thinking together with people who have lived/living experience of mental health issues to work out how best to address these issues for people.
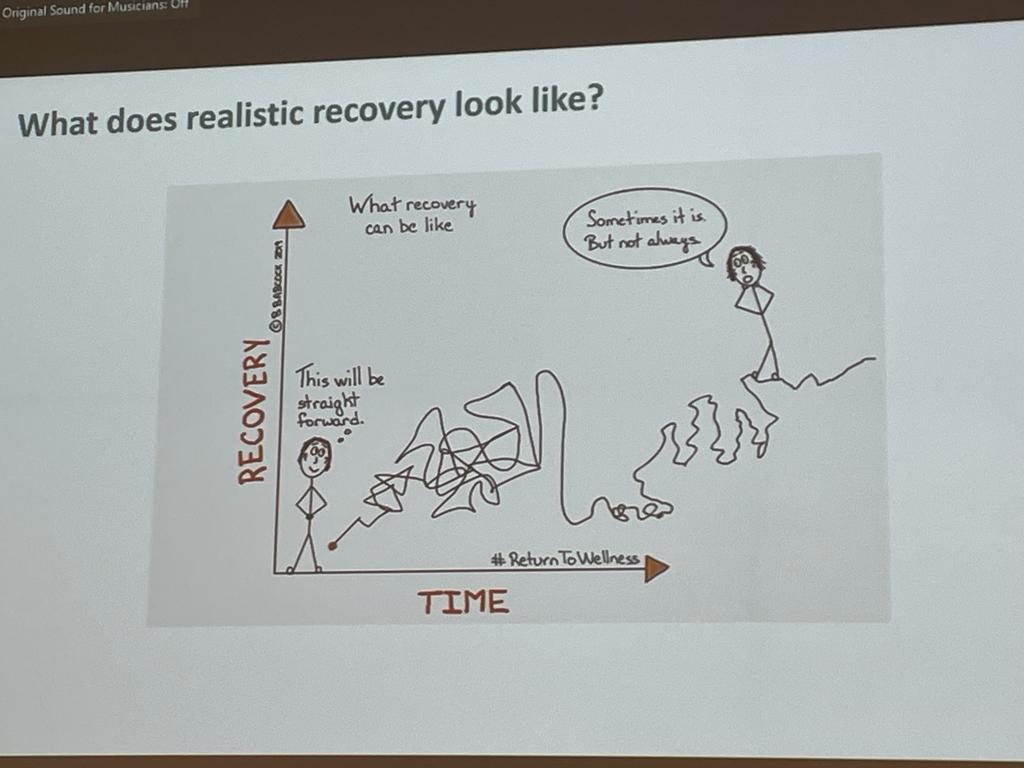
Recovery is not a linear journey….
Joe Firth
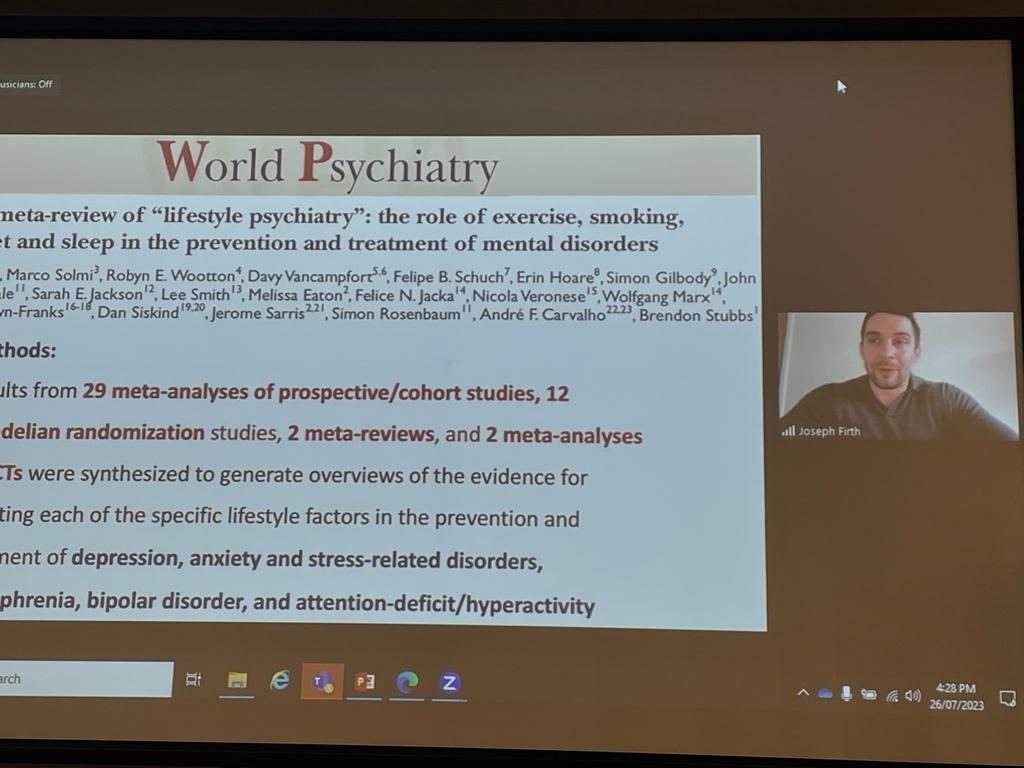
Dr Joe Firth (University of Birmingham) graced us with his charm as he gave an exposé of his published work ranging from The Lancet Psychiatry’s Blueprint on protecting the physical health of people with mental illness (called “The Blueprint” available here), to his meta-review of lifestyle psychiatry published in World Psychiatry (here). Joe is a ‘lad’ from the Manchester who loves a bit of mixed marital arts, and is reputed to have single-handedly propped up an unnamed university by a rung or two in the global rankings with his exceptional publication record.
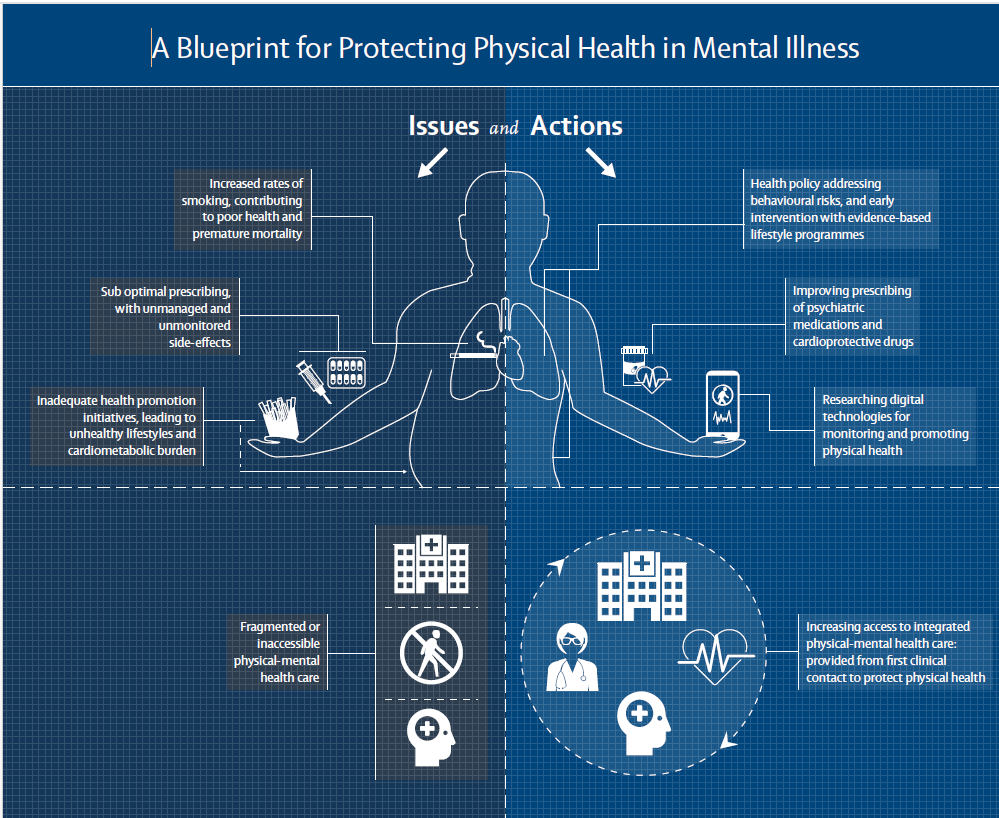
The Lancet Psychiatry Commission’s Blueprint for protecting the physical health of people with mental illness (led by Joe Firth)
The Blueprint spans primary prevention, initial treatment and continuing care, and considers global systems. Promising areas for future research include implementation of physical health interventions in routine care, including investigating the use of digital technologies, and preventative lifestyle intervention programs. Technology holds promise for increasing engagement. Apps can increase engagement and support behaviour change for quitting smoking, increasing physical activity, and making other lifestyle changes.
Exercise programs should be group based, and can improve symptoms of many mental health conditions. A recent randomised controlled trial (available here) with over 200 participants demonstrated that a 6-month general lifestyle intervention can reduce weight for people with severe mental illness. Studies incorporating wellbeing and cost-effectiveness outcomes are needed. Mental health settings need a greater presence of professionals who focus on physical healthcare to drive these improvements and support culture change.
Joe Firth presenting online about lifestyle interventions and mental health
Livia De Picker
Dr Livia De Picker has led work in Europe to protect people with mental illness against COVID19. The first reports of heightened risk of infection and mortality caused by COVID19 in people with severe mental illness were available in September 2020. However, this wasn’t effectively considered in determining vaccine access to priority groups across Europe. Policy makers were not aware of the risks, mental health representatives were not involved in decision making, and stigmatising or misinformed attitudes likely underpinned lack of action. After their press campaign to disseminate knowledge about increased risk, gradually countries began taking action.
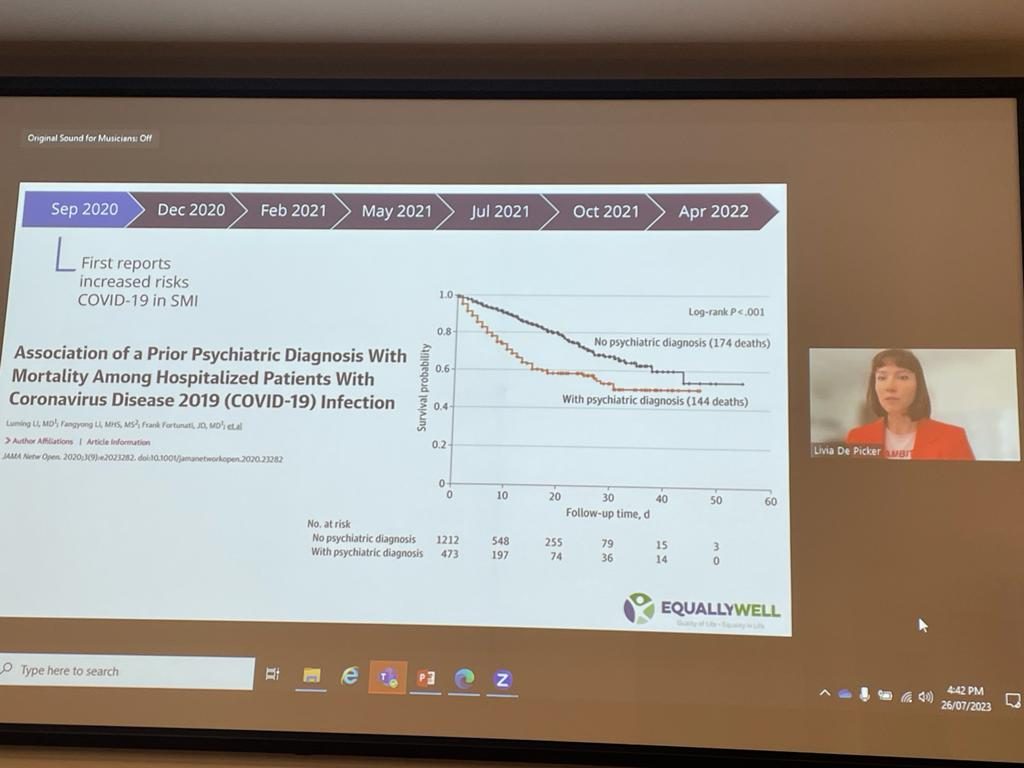
Livia De Picker presenting online about COVID19 mortality in people with mental illness
In May 2021, Livia’s meta-analysis in Lancet Psychiatry demonstrated a two-fold increased risk of mortality caused by COVID19 in people with any mental health condition, and this risk was highest in people with psychoses. ‘Lags’ in rates of being vaccinated were also observed for people with severe mental illness, so barriers to access need to be addressed. By distributing vaccines to people receiving mental health care in hospitals, they enabled mental health workers to provide the vaccine directly to consumers, which increased vaccination rates. This indicates that it was not ‘vaccine hesitancy’ as many people thought, but simply barriers to accessibility.
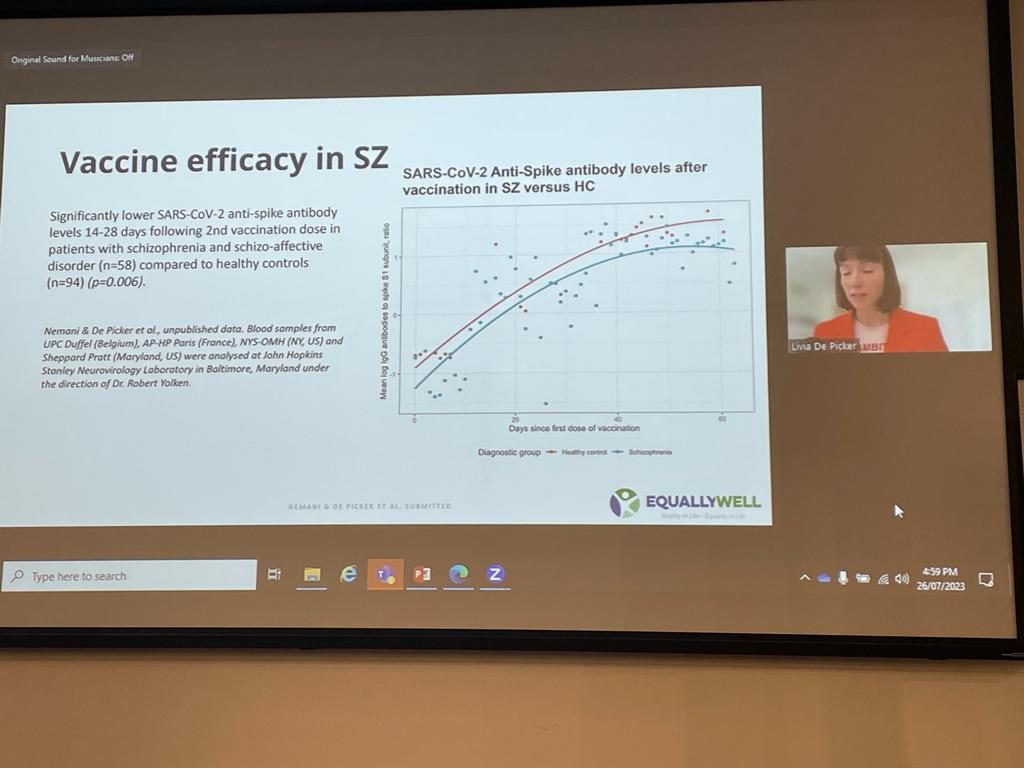
Livia De Picker presenting online about vaccine efficacy in people with mental illnesses
Beyond the pandemic, we are still seeing higher rates of preventable deaths in people with severe mental illnesses. Their recent study demonstrated lower vaccine response in people with severe mental illness because they produced a lower level of antibodies, which may be related to reduced vaccine efficacy. Proactive approaches to vaccine equity for people with mental illness is needed, and research in this area needs to be prioritised.
Day three: 27th July 2023
Arriving right on time for the last day (and as they say, if you’re not early you’re late), I must admit I’m feeling a bit exhausted (and think I may have RSI after all this typing). As a mere human, my ‘cup’ is about full after being crammed full of information from this incredible symposium. Whenever I feel like I’ve hit a wall I tend to get introspective, and there’s no better way to contemplate my humanity then to take a stroll through the Out from the Mist exhibition. Although the artists who submitted these images to the competition (which is still open to all humans, so get your entries in) no doubt intended a much deeper meaning, I found the below images quite reflective of my feelings after these last couple of days.
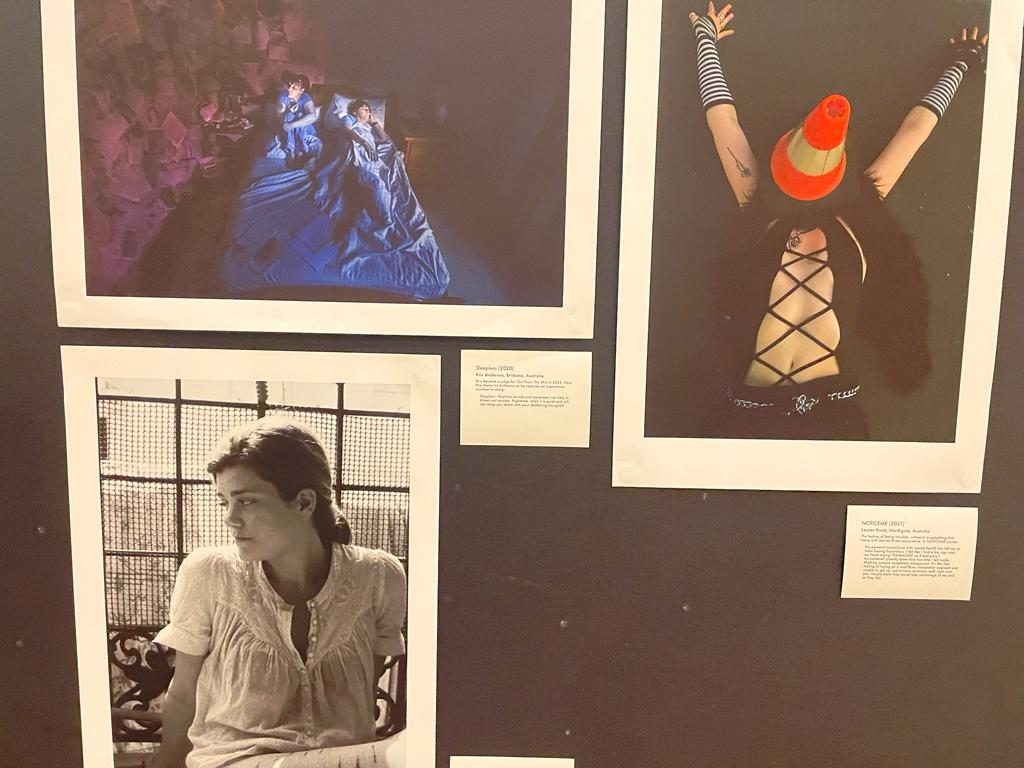
Out from the Mist submissions: Sleepless by Kris Anderson (top left); NOTICEME by Lauren Knott (right); The Pattern by Anouk Pistolesi (bottom left)
Emily Unity
First up, we had an address from Emily Unity (they/them), who strives to bring humanistic approaches into mental health services and everyone’s lives. Emily brings her lived experience into her work, and has made waves in advocating for mental health, diversity and equality (and is also a software engineer and designer, so I recommend taking a look at her personal page)
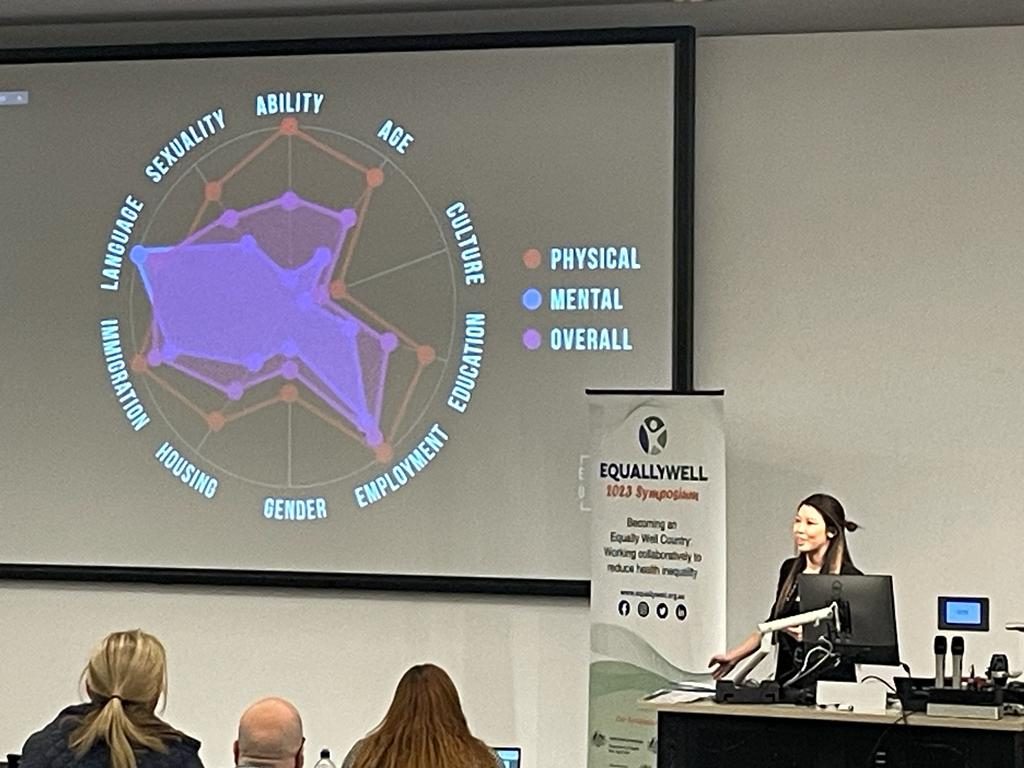
Emily Unity giving an excellent overview of her experience with inequity, and the multitude of influences that make up our identity and life experiences
Emily spoke about intersectionality, and the invisibility of mental health conditions. Misdiagnosis and invalidation of people’s experiences can be common because of the subjective nature of mental health challenges. To demonstrate how our preconceptions form the [incomplete and often biased] lens through which we make judgements, Emily plotted different components of ‘privilege’ and ‘disadvantage’ which highlighted the spectrum of biopsychosocial determinants that influence our life trajectories. Without knowing a person’s full story it’s impossible to make accurate judgements. Treating people holistically and openly communicating with consumers is a consistent theme in this conference.
Grant Sara
Dr Grant Sara, recent Equally Well award recipient and Director of InforMH (NSW Ministry of Health) followed up with a great overview of how to see the human story among the data. Grant pointed out that there is lots of evidence that there is a problem, but less evidence about how to change it. “In tackling these big problems, we need a whole range of perspectives”.

Dr Grant Sara presenting on his work in making best use of the data
There are big data gaps that Grant and his team are trying to close by linking databases across the fragmented services of community mental health, emergency, hospital care, physical health services etc. Ideally, data will be local, detailed, recent and actionable to support health system change. One of these projects is about cancer screening: they found that women with mental health issues are only 74% as likely to be screened for cervical cancer as the general population, a screening gap which is greater for older women. Screening rates vary by health district; however, all districts had a gap in screening rate between mental health consumers and others.
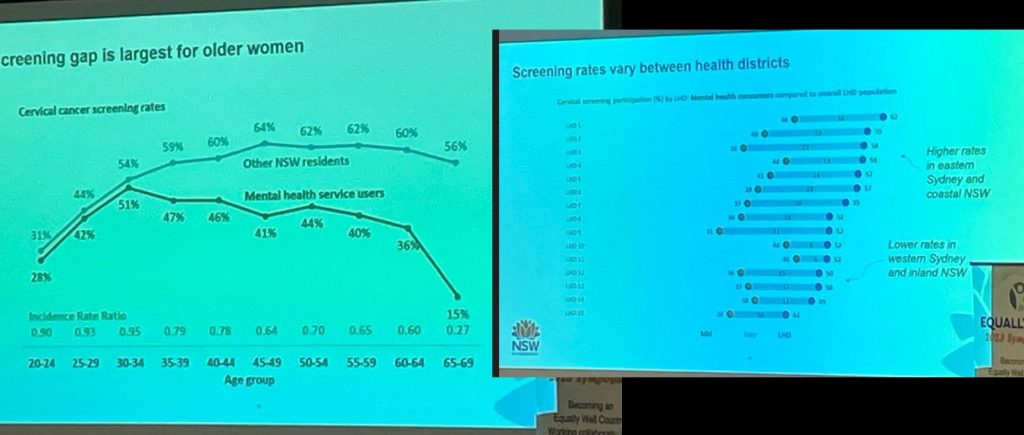
The gap in cancer screening rates and preventable hospitalisations between people with mental health issues and others
Grant also presented on hospitalisation rates, finding that people who use mental health services were 2.6 times more likely to be hospitalised as a ‘potentially preventable hospitalisation’ (PPH), and to have a 39% longer hospital stay. When considering causes, alarmingly, 29% of hospital bed days were because of nutritional deficiency. These statistics has prompted their team to work more closely with dietitian superstar Dr Scott Teasdale to improve food security for people with mental health issues.
Grant’s take home messages were that life expectancy is an important indicator, but limited on its own. There are big gaps in data which makes understanding the full spectrum of care difficult (e.g. medications etc), and understanding individuals’ cultural, family and personal context very difficult. Data on its own doesn’t lead to change, but can be useful for informing actions and measuring progress. Grant’s advice to mental health services was to “Look at your data know and identify where you need to act“.
Concurrent sessions
Then we split into concurrent sessions; topics were Focused initiatives, Vulnerable populations, Engagement & physical activity, and Continuity of care. In times like these I wish I could be omnipresent like Dr Manhattan from Watchmen, but unfortunately I once again had to acknowledge my limitations as a human, and attend only one stream of presentations.
Dr Manhattan from the 2009 film Watchmen could be in multiple places at once, an ability that could be put to good use for learning about everything that everyone presented at Equally Well Symposium 2023
Follow Laura on The Mental Elf’s twitter account for an update on the Vulnerable populations stream here.
Justin Chapman and Ailsa Rayner
Personally, I’m a card-carrying physical activity activist (you can see one of my other blogs with The Mental Elf here) and chose to attend the Engagement & physical activity stream… also I had present my own work in this stream, so my coverage of that presentation may be somewhat biased.
Dr Justin Chapman is a Research Fellow with Griffith’s Centre for Mental Health and the Translational Mental Health and Co-design Research (ITHACA: a prize for anyone who work out where these acronym letters come from) group led by Professor Amanda Wheeler, Board member of Psychosis Australia who are holding the Australian Psychosis Conference back here in Sydney in September, Senior Peer Research Officer at Metro South Addictions and Mental Health, and Research Fellow with the ALIVE National Centre. Although not delivering a very noteworthy presenting, I decided to give it a red-hot crack and say a few things about how great exercise is for improving mental health and recovery.

Irene McCarthy took some photos with her Nokia brick phone from 2001: Justin Chapman (left) and Ailsa Rayner (right) presenting on Healthy Lifestyle Programs delivered by PCYC Queensland in partnership with MIND Australia.
I was delighted to also have Ailsa Rayner co-present, who provided insights into the success stories (published by the North Queensland Primary Health Network) as a co-facilitator of the program with Jane Kugelman, you can see her adventures here (posted with permission).
Matt Fluder and Elena Walker
Matthew Fluder and Elena Walker have co-designed and implemented the Walking toward Wellness program at Wellways. Matt quoted “The Baum” who said “we need to address physical health as a priority, and we need programs with efficacy in the community”. The program is based on motivational theory, and has shown improvements after six weeks in emotional connection and self-efficacy. Elena (Senior Peer Rehabilitation and Recovery Worker) began by recognising the contributions of lived experience and their family and carers, and acknowledged the impact that mental ill-health can have on physical health.
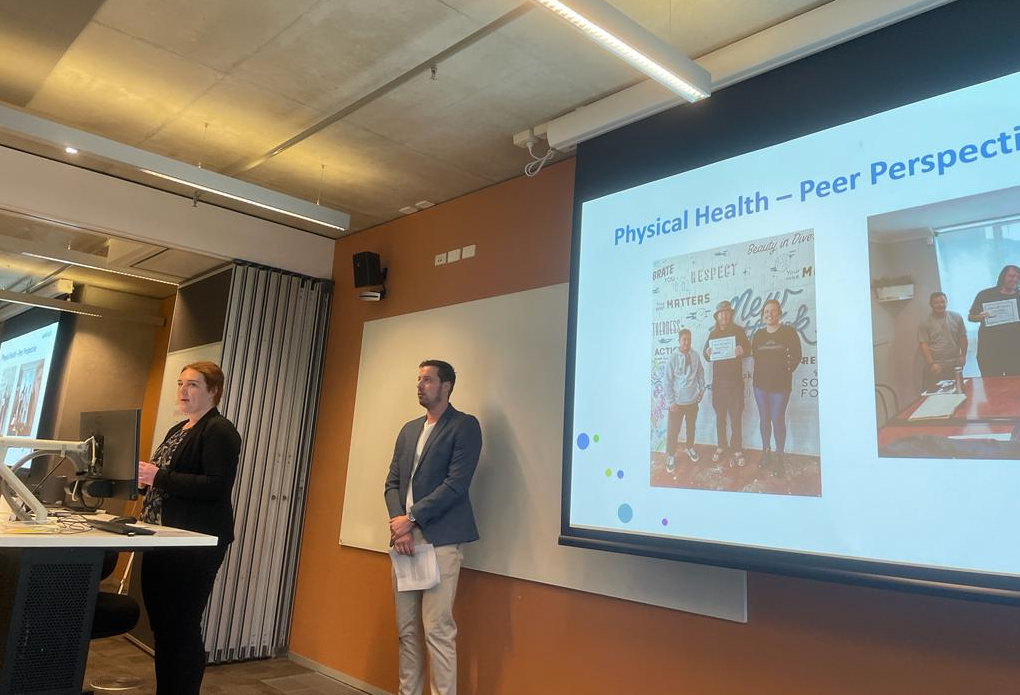
Elena Walker (left) and Matthew Fluder (right) presenting on Walking toward Wellness
People with mental health issues need to be empowered to make incremental progress, and afforded the opportunity of a recovery-oriented program like Walking toward Wellness. A non-judgemental forum for constructive conversation and connection with like-minded people is an essential platform for engagement in such programs.
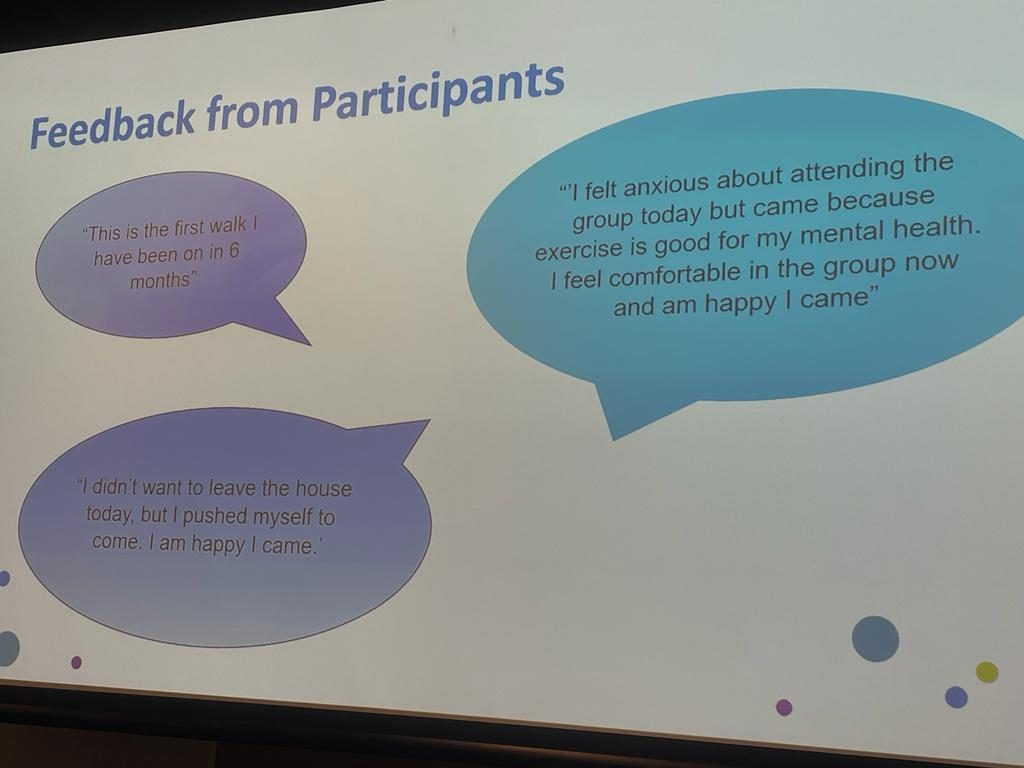
Participant feedback from Walking toward Wellness
Participant feedback was that the program approach improved confidence, which generalised into other aspects of their life. You can hear about their work on the Brainwaves podcast here.
Phoebe Connors and Antoinette Tipple
Next up we heard from Phoebe Connors and Antoinette Tipple who presented a co-designed Healthy Me, which involves group-based exercise and healthy eating sessions delivered by an exercise physiologist.
Phoebe Connors (left) and Antoinette Tipple (right) presenting on Healthy Me
The program is goal oriented and addressed priorities outlined in the National Preventative Health Strategy to support people with mental health issues make healthy lifestyle changes, and is based on the Stages of Change model. Healthy Me fosters a ‘club’ mentality, and includes prizes for engagement which can be important for promoting motivation when people just aren’t feeling like jumping out of bed that day.
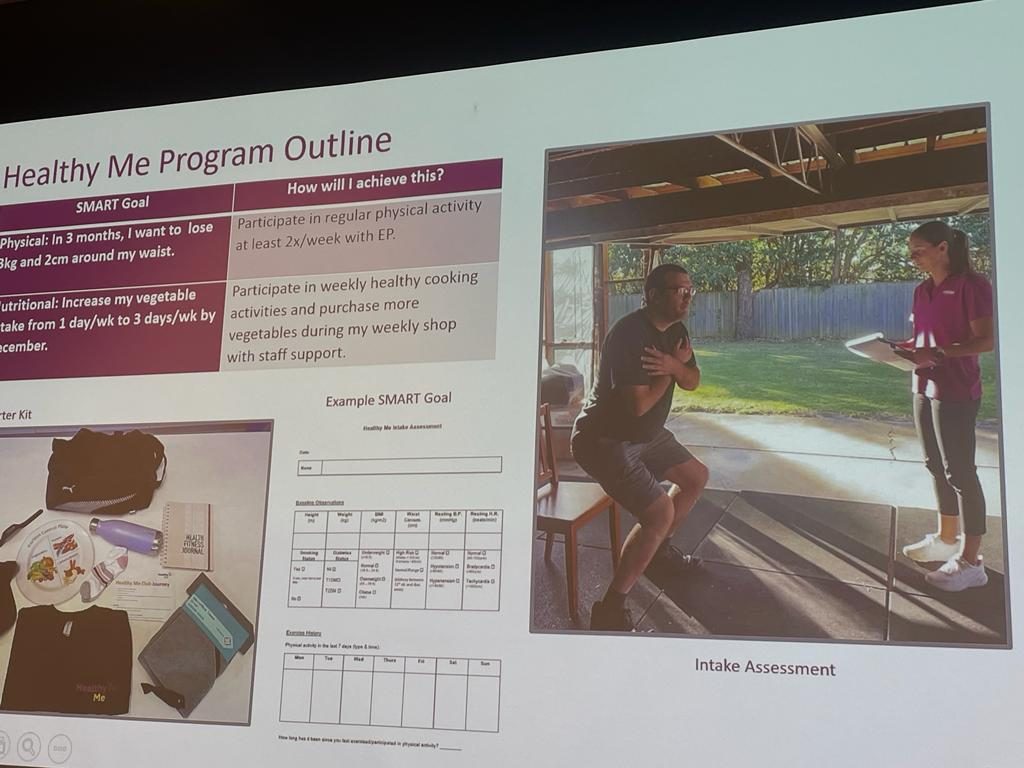
Elements of the Healthy Me program
Lessons learned included that the group environment is essential, with participants connecting and providing social support. The club will continue to be co-designed to ensure it’s meeting people’s physical health and wellbeing needs.
Tegan Stettaford
Tegan Stettaford is a proud PhD candidate at the University of Newcastle, who presented preliminary qualitative findings from her telephone service for lifestyle coaching. Telephone coaching can be effective for people with mental health issues, and through Tegan’s PhD work, the Get Healthy Service has demonstrated positive impacts.
Tegan Stettaford presenting on her PhD work in telephone coaching.
People reported that their sense of self was holistic, and their physical and mental health could not be separated. The flexibility of the service was a key feature that people enjoyed, and the text message prompts to motivate and remind people to keep going was valued. However, sometimes the appointments felt too rigid and easy to ignore for some people when things became difficult. The relationship between the coach and participant was the key ingredient for supporting people, and when the coach recognised participants as the experts in their lives, people felt supported and part of a safe space.
Terry Slevin
Then we returned to the Main Auditorium for the final Keynote speaker, Professor Terry Slevin, Chief Executive Officer of the Public Health Association of Australia (PHAA). Terry acknowledged Country, and began with a disclaimer stating that he’s not a mental health expert, but brings a Public Health Toolbox to his work. Getting action in Government is tough because there’s enormous competition for attention and resources. Terry commended Equally Well for the enormous progress we’ve all made over the last 10 years.
Professor Terry Slevin presenting on a public health approach to mental health
The COVID19 pandemic stimulated an increase in government funding on health. However, the pandemic of chronic disease is easily ignored despite causing a significant cost to the health system and negatively impacting people’s lives on a broad scale. Focusing on people experiencing marginalisation is essential to ensure everyone receives the same level of care and has equivalent opportunity to live productive and fulfilling lives. But to secure increased investment, we have to ‘sell’ the idea. To bring mental health along with the priorities of public health improvement and prevention, we need to focus on the whole population AND establish what we need to do differently for people with mental health issues. Social and societal norms drive behaviour, so focusing on a specific sub-group of the population is fraught, and a whole-of-population approach is necessary.
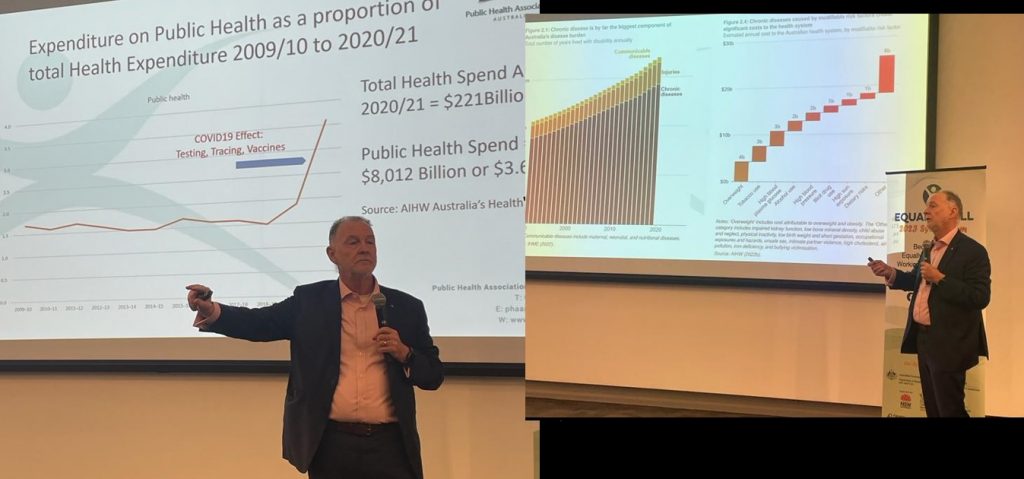
Terry presenting on the impact of COVID19 with chronic disease investment
Terry commented on the Equally Well Consensus Statement and suggested that a broader focus is needed. To take a broader lens, we could focus on what happens before first contact with mental health services in our promotion, prevention, and early intervention strategies. Good public health policy is not always easy or popular, but a societal approach is needed to reduce availability of unhealthy choices and enable healthier choices by targeting the context in which we live. A national shame in Australia is the gambling culture and the public policy failure to address it. The financial interests at stake cause corrupted decisions at the highest levels, which has a substantially negative impact on Australia’s most vulnerable. This is also a mental health issue.
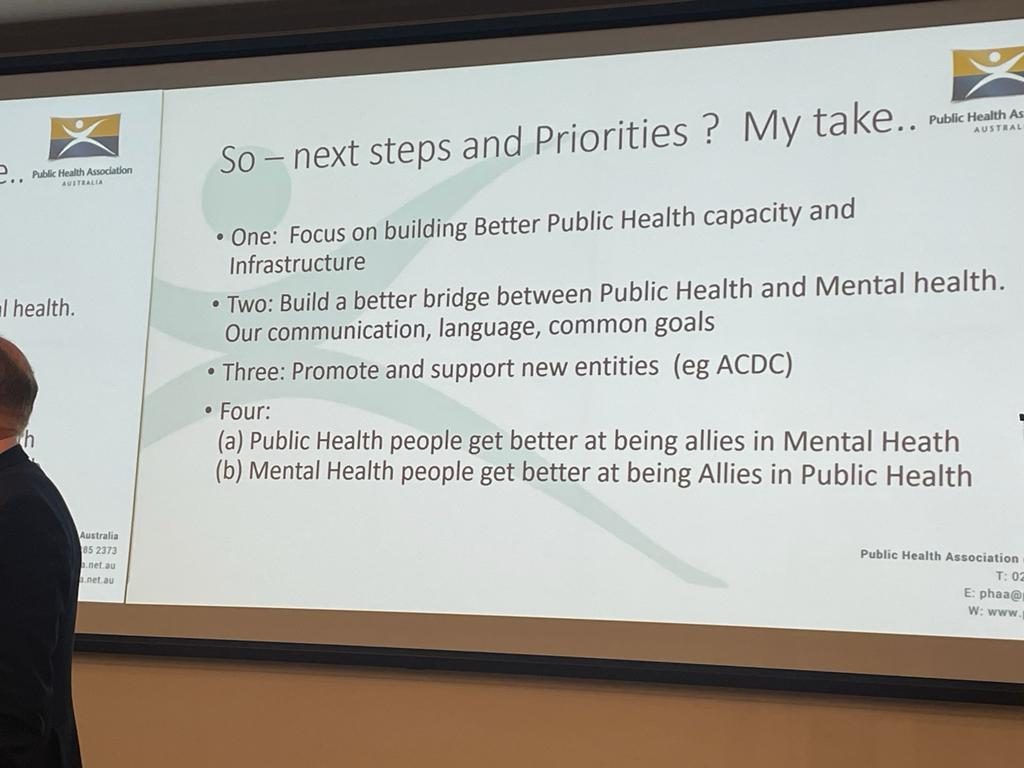
Terry’s take-home messages
Measuring what Matters is our first national wellbeing framework. However, the progress we are able to make is dependent on the resourcing decisions made at strategic levels. We need to find ways of providing input to the decision-making process to sharpen funding to make the biggest impact. There’s an important opportunity for the mental health sector to leverage this development and guiding implementation strategies. We need to focus on building better public health capacity and build a better bridge between public health and mental health.
Closing comments
Johan and Dave gave us a high-level overview of the last couple of days. Key themes were intersectionality, and how to make meaningful use data. John acknowledged that the Equally Well symposiums have evolved over time and improved in sophistication, and we can now enjoy less whinging about problems, and more positive messages about actions and achievements. Dave thanked everyone for their involvement and contribution, especially the Equally Well team for organising the event. And we couldn’t finish without a final address from Australia’s favourite man!

Russell, John and Dave wrapping up the symposium events
Finally, I got to catch up with the Powerhouses behind the Equally Well symposium, Victoria, Lee and Skye:

