
The diagnosis and treatment of apical periodontitis can be complicated, especially if it is asymptomatic or has complex radicular architecture, and not all apical radiolucencies are inflammatory lesions. Conventional two-dimensional (2D) radiography is the most common imaging technique to identify these lesions, but it cannot always detect every apical lesion due to its size or the presence of other anatomical structures. Cone-beam computed tomography (CBCT) adds a third dimension to the image (3D), allowing the clinician to visualise the true extent of a periapical lesion in the horizontal plane. However, this improved diagnostic yield comes at both a cost in additional radiation exposure and overall cost to the patient.
The aim of this study was to compare the diagnostic performance outcomes between conventional 2D radiographs and CBCT in detecting persistent apical disease after root canal treatment. (Ramis-Alario et al., 2021)
Methods
The study followed the Preferred Reporting Items for Systematic Reviews and Meta-analysis for Diagnostic Test Accuracy (PRISMA-DTA) guidelines. Two independent authors conducted an electronic search of the Medline via PubMed, Embase, Web of Science and Google Scholar databases for published articles up to December 2019 without language restriction. Opengrey was also searched for non-peer reviewed literature. The risk of bias was assessed using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) guidelines.
Results
- Of the 27 papers, 13 articles compared digital periapical radiography (DPR) vs CBCT, two articles compared conventional periapical radiography (CPR) and DPR vs CBCT, two compared DPR and panoramic radiography vs CBCT, five compared CPR vs CBCT, one compared CPR and panoramic radiography vs CBCT, one compared periapical radiography vs CBCT but failed to mention the features of both CBCT and periapical x-ray devices, and three articles compared panoramic radiography vs CBCT.
- The risk of bias was high in terms of flow and timing but low in terms of applicability.
- Primary diagnostic measures
- Sensitivity and specificity for 2-D radiograpgy compared to CBCT. The pooled sensitivity and specificity estimates were 58% (0.58; 95% confidence interval (CI), 0.53 to 0.64) and 100% (1.00; 95% CI, 1.00 to 1.00), respectively.
- The overall heterogeneity was high for sensitivity (I2 = 97.3%).
- The pooled area under the receiver operating characteristic curve (AUCROC) discriminating capacity of conventional radiographs to diagnose persistent apical disease was good at 77% (0.77; 95% CI, 0.75 to 0.80).
- Secondary diagnostic measures
- Positive and negative predictive values. The pooled positive predictive value estimate was 100% (1.00; 95% CI, 1.00 to 1.00; data not shown). The negative predictive value was 68% (0.68; 95% CI, 0.63 to 0.72)
Conclusions
The authors concluded:-
Moderate certainty evidence suggested that conventional radiographs showed poor sensitivity and excellent specificity but good diagnostic performance in terms of AUCROC and accuracy. Sensitivity, AUCROC, and negative likelihood ratio values could be reduced if the time elapsed to diagnosis after root canal treatment exceeded 5-years. The use of CBCT with a reduced field of view or a 2D radiographic technique should be weighed considering patient-specific and indication-oriented criteria as taking precedence over the therapeutic goal.
Comments
This review followed the standard PRISMA-DTA protocol but lacked pre-registration; however, it had a large sample size for meta-analysis and opens up some interesting areas for discussion regarding the cost in terms of harms and benefits of achieving increased diagnostic yield in imaging. To refine the comparison of 3D with 2D radiography, I will limit the discussion to CBCT compared with digital periapical radiography. To add some context, there was a recent paper published comparing CBCT with intraoral periapical lesions in endodontics which concluded that: –
CBCT imaging was reported in this investigation to have twice the odds of detecting a periapical lesion than traditional periapical radiography in endodontic outcome studies.(Aminoshariae et al., 2018)
It can sometimes be quite challenging to interpret odds ratios as they are not the only way to present an association when the primary outcome is binary. The reader should understand odds ratios in the context of other information, such as the underlying probability (Norton et al., 2018). I have taken the primary data from Aminoshariae and redone the meta-analysis to show the risk difference rather than the odds ratio (Figure 1).
Figure 1.
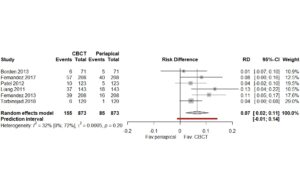 From these new results, we can see that there is a small but significant increase in the ability of the CBCT to detect apical pathology of 7% (95%CI: 2% to 11%: Prediction interval -1% to 14%), which appears less dramatic than the also correct doubling of odds (2.04 (95%CI: 1.52 to 2.73). Since the improvement was significant, CBCT was selected as the reference standard for the Ramis-Alarios paper. As the pooled analysis contained a mix of conventional, digital intraoral, and panoramic radiographs, I have calculated a new Summary Reciever Operating Characteristic (SROC) curve using the ‘mada’ package in R. Only the primary data regarding digital periapical radiography data was used. There were zero false positives in the data, so a continuity correction of 1 had to be applied to plot the new SROC curve, which sightly reduced the specificity from 100% to 96%. The new summary estimate for digital periapical radiography produced a sensitivity of 58.5% (95%CI: 48% to 68%) and a specificity of 96% (95%CI: 98% to 93%), the AUCROC was excellent at 0.90 (Mandrekar, 2010) (Figure 2.).
From these new results, we can see that there is a small but significant increase in the ability of the CBCT to detect apical pathology of 7% (95%CI: 2% to 11%: Prediction interval -1% to 14%), which appears less dramatic than the also correct doubling of odds (2.04 (95%CI: 1.52 to 2.73). Since the improvement was significant, CBCT was selected as the reference standard for the Ramis-Alarios paper. As the pooled analysis contained a mix of conventional, digital intraoral, and panoramic radiographs, I have calculated a new Summary Reciever Operating Characteristic (SROC) curve using the ‘mada’ package in R. Only the primary data regarding digital periapical radiography data was used. There were zero false positives in the data, so a continuity correction of 1 had to be applied to plot the new SROC curve, which sightly reduced the specificity from 100% to 96%. The new summary estimate for digital periapical radiography produced a sensitivity of 58.5% (95%CI: 48% to 68%) and a specificity of 96% (95%CI: 98% to 93%), the AUCROC was excellent at 0.90 (Mandrekar, 2010) (Figure 2.).
Figure 2.
The subgroup analysis concluded that digital periapical radiography displayed an excellent diagnostic capacity when compared to CBCT. Therefore the small increase in diagnostic accuracy offered by the CBCT needs to be weighed against the increased effective dose of radiation the patient will be exposed to yield that additional information. To clarify this point a single digital periapical radiograph has an effective dose of 0.005mSv ( 1 day of background ). A current CBCT set at a high resolution for endodontics will have an effective dose ranging from 0.041mSv to 0.143mSv ( 8 to 29 days of background radiation)(Qiang et al., 2019; White et al., 2014). To quote Ramis-Alario:
“The decision to use CBCT or a 2D technique in patients in whom a functional tooth exhibits a periapical radiolucency after conventional root canal treatment should be clearly justified by the clinician to avoid unnecessary radiation exposure to the patient, in keeping with the “as low as diagnostically acceptable” (ALADA) criterion.”(Ramis-Alario et al., 2021)
Links
Primary reference
Other references
Aminoshariae A, Kulild JC, Syed A. Cone-beam Computed Tomography Compared with Intraoral Radiographic Lesions in Endodontic Outcome Studies: A Systematic Review. J Endod. 2018 Nov;44(11):1626-1631. doi: 10.1016/j.joen.2018.08.006. PMID: 30409446.
Mandrekar JN. Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol. 2010 Sep;5(9):1315-6. doi: 10.1097/JTO.0b013e3181ec173d. PMID: 20736804.
Norton EC, Dowd BE, Maciejewski ML. Odds Ratios-Current Best Practice and Use. JAMA. 2018 Jul 3;320(1):84-85. doi: 10.1001/jama.2018.6971. PMID: 29971384.
Qiang W, Qiang F, Lin L. Estimation of Effective Dose of Dental X-Ray Devices. Radiat Prot Dosimetry. 2019 Jun 1;183(4):417-421. doi: 10.1093/rpd/ncy159. PMID: 30169836.
White SC, Scarfe WC, Schulze RK, Lurie AG, Douglass JM, Farman AG, Law CS, Levin MD, Sauer RA, Valachovic RW, Zeller GG, Goske MJ. The Image Gently in Dentistry campaign: promotion of responsible use of maxillofacial radiology in dentistry for children. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014 Sep;118(3):257-61. doi: 10.1016/j.oooo.2014.06.001. Epub 2014 Jun 16. PMID: 25066244.
Picture Credits
Photo by Jonathan Borba on Unsplash


For clinical relevance, given the safety issues for routine use of CBCT, it would be helpful to know the specificity performance between diagnosis using these images when augmented intelligence is applied to each form of image
The use of AI to facilitate diagnosis is an interesting area for future study. At present, there is a high degree of variability in AI models under investigation and we will need some very high quality large studies to draw a robust conclusion. In a paper called ‘Evaluation of artificial intelligence for detecting periapical pathosis on cone-beam computed tomography scans by Orhan et al 2020 the author concluded that ‘Volumetric measurements created by a manual segmentation method and by an AI system were comparable to each other’. Though sensitivity may be high it may be interesting to see in the future what the false positive rate would be – specificity could be quite low as has been found in other areas – ‘Comparison of performances of artificial intelligence versus expert endoscopists for real-time assisted diagnosis of esophageal squamous cell carcinoma (with video)’ Fukuda et al.2020