
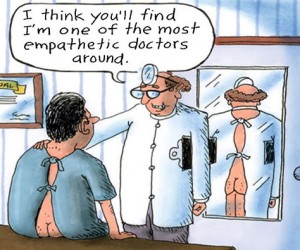
When I started to write this blog I used the age-old tactic from schooldays of having the TV on in the background to “help my concentration”. And then I got distracted by a comedy featuring – you guessed it – a stupendously un-empathic doctor. How weird is that? It’s spooky being an Elf sometimes.
One would always hope for, although sadly not necessarily expect an empathic doctor. To be honest, I’m usually quite grateful if they’re not young enough to be my daughter or son. Whilst medical education in most cultures explicitly emphasises the importance of empathy, there is evidence that this desired characteristic declines during medical education, and is “lower than ideal” in physicians.
Studies indicate that doctors overlook or miss empathic opportunities in patient encounters.
Methods
I have to confess, I rolled my eyes when I first read the title of this review – Interventions to cultivate physician empathy: a systematic review (Kelm et al, 2014). I was being rather unfair as it turned out. It’s definitely a very worthwhile question to ask, and I was actually quite surprised to learn that this was the first review comparing quantitative evaluation studies on the subject.
I was also impressed with the methods the researchers used and the logic and clarity of the reporting. Not only did they have a librarian’s help in designing the literature search strategies (although as usual, they only considered studies written in English), they also explicitly reported their adherence to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta Analyses) guidelines. As I work for the EQUATOR (Enhancing the QUAlity and Transparency Of health Research) Network, an organisation dedicated to promote the use of reporting guidelines, it was heart-warming to see.
Inclusion criteria were studies where:
- Intervention was designed to cultivate empathy
- Empathy was evaluated using quantitative outcome measures, and statistical analysis
- The population were qualified doctors or medical students

Explicit adherence to PRISMA guidelines engenders a feeling very much like quaffing a rum hot chocolate on a wintery Sunday afternoon.
Results
Types of intervention
The interventions designed to cultivate empathy were of several types:
- Communications skills training interventions were used in nearly a third (20) of the studies, and usually consisted of a mixture of lectures, videos, experiential workshop training such as practice interactions using role play and feedback.
- Around a tenth of the studies (seven) primarily used role play with study participants acting as patients. For example one study had medical students injecting each other with saline solution.
- Another tenth of the studies (six) were described as using “humanities”, which included reflective writing from the patient point of view and theatre.
- Three studies used balint training which involves small group discussions focussed on patient emotions.
- Two studies used mindfulness-based stress reduction (MBSR), a type of meditation characterised by non-judgmental, moment-to-moment awareness.
- One study used problem-based learning sessions focussing on empathy and communication.
- Over a third (23) of the studies mixed a variety of interventions so these could not be easily categorized, although they consisted mostly of communication skills training interventions.
Characteristics of included studies
Sixty-four studies met the inclusion criteria and data on ten metrics were extracted from each including:
- Study size and time frame of outcome assessments.
- Whether a control group and random assignment was used.
- The validity of the outcome measures.
- Whether or not a statistically significant increase in empathy was reported.
The statistical significance thing worried me a bit. Unless researchers in each study have specified and justified the minimally useful effect size to a patient-relevant outcome, statistical significance doesn’t necessarily mean that the intervention would make a useful difference in real life.
Quality of the evidence
The researchers also graded the 64 studies into three tiers of methodological quality, and only ten studies made it into the top tier. Of those ten methodologically rigorous studies, eight found that the intervention had a statistically significant positive effect on empathy.
Overall, the percentage of studies reporting a significant positive effect was 66%, although as previously mentioned the studies as a whole were characterised by poor design, inadequate reporting, and the time-frame of follow up was mostly very short or immediate. The studies were mostly small, and vague descriptions of interventions mean they cannot be replicated in further evaluation research, or put into practice.
Patient-reported outcomes
Only six of all the studies (9%) measured patient reports of empathy, despite the existence of reliable and valid patient-report measures. Having read the review quite carefully, all I really wanted to find out was which studies reported a significant increase in empathy using patient-reports, and had a follow-up of more than a few weeks – in other words, any studies which vaguely approached real life. I dug around in the additional tables just in case, and alas there were none.

Remarkably few of the included studies measured patient reports of empathy, which makes it hard to apply the findings to real life.
A final note
As you’ve read this far, I’d recommend you take an extra ten minutes to watch an inspiring video made by the Canadian Patient Safety Institute. It’s a mother’s moving story in her own words which perfectly illustrates how important it is for healthcare providers to take just a little time to try and understand every patient’s perspective. In particular, her courageous intervention on behalf of her daughter taught one doctor what I am sure was an invaluable and lasting lesson in empathy. That is what I call a significant result.
Link
Kelm Z, Womer J, Walter JK, Feudtner C. (2014) Interventions to cultivate physician empathy: a systematic review. BMC Medical Education 2014; 14(1): 219. doi:10.1186/1472-6920-14-219.


Marigolds or orchids? How easy is it to cultivate empathy in doctors?: Caroline Struthers takes us through a r… http://t.co/mqmIi2oH4f
RT @Mental_Elf: Marigolds or orchids? How easy is it to cultivate empathy in doctors? http://t.co/JlKzauCedW
Marigolds or orchids? How easy is it to cultivate empathy in doctors? http://t.co/x1qB8ozagU via @Mental_Elf
Olivia Cialdi liked this on Facebook.
#ActuSanté – Marigolds or orchids? How easy is it to cultivate #empathy in #doctors ? @ALOISCommunity http://t.co/kZ0TwZkcPP @Mental_Elf
Today @ALOISCommunity looks at a systematic review of interventions to cultivate physician empathy http://t.co/JlKzaukDmo
@Mental_Elf @ALOISCommunity Does the decline in empathy just happen or is it cultivated?
Hi there @hermitsholiday @Mental_Elf . According to the review it is caused by stress and burnout
Truly excellent @Mental_Elf blog on cultivating empathy in doctors. Read the blog, but DONT skip the video!
http://t.co/dpNvOKXsrX
How easy is it to cultivate #empathy in doctors? Via @Mental_Elf http://t.co/DT2SkHs0vq
“Studies indicate that doctors overlook or miss empathic opportunities in patient encounters” The latest evidence: http://t.co/JlKzaukDmo
@Mental_Elf @learnhospice might be useful?
@amdickinson1 @Mental_Elf TY Angie: yes v interesting in the dominant teaching & evaluation methods quandary
The Mental Elf liked this on Facebook.
Why do studies of physician empathy not measure patient reports of empathy? http://t.co/JlKzaukDmo #ObviousPlaceToStart
Marigolds or orchids? How easy is it to cultivate empathy in doctors? http://t.co/m09PQ1zfX5 @mental_elf #hcldr #hcsm @colin_hung @nxtstop1
@StuckonSW @Mental_Elf @Colin_Hung Thanks~Super article-Sadly couldn’t download video. The patient side of the equation is what matters.
@nxtstop1 @Mental_Elf @Colin_Hung thought you would enjoy it. Video worked for me??
@StuckonSW @Mental_Elf @Colin_Hung Thx 4 telling me > I’ll try PC
Marigolds or orchids? How easy is it to cultivate empathy in doctors? http://t.co/9WOPfLGg2j via @sharethis
RT @Mental_Elf: Hi @Patient_Safety We’ve included your amazing video https://t.co/Hlqeb2qLnP in our blog about physician empathy http://t.c…
@Mental_Elf blog on new sys review praises authors’ explicit use of @PRISMAStatement http://t.co/lHvZwVjr3o#sthash.B8FxSCE8.dpuf
Mental Elf: Marigolds or orchids? How easy is it to cultivate empathy in doctors? http://t.co/yreKmXi49K
Marigolds or orchids? How easy is it to cultivate empathy in doctors? http://t.co/2gxNpYNMuF TY @Mental_Elf http://t.co/i6RLBRxnPd
Marigolds or orchids? How easy is it to cultivate #empathy in medical #doctors? http://t.co/0DM3Dkcgxi
Don’t miss: Marigolds or orchids? How easy is it to cultivate empathy in doctors? http://t.co/JlKzaukDmo
Christina Armstrong-Graham liked this on Facebook.
Marigolds or orchids? How easy is it to cultivate #empathy in #doctors? http://t.co/A4lHjSmoCf @Mental_Elf reports on a #systematicreview
Can doctors do Empathy http://t.co/LSmwDGU0SX
I have been a healthcare professional for over 25 years and I have also been a recipient of mental health care during that time. So I have been on both sides of the healthcare fence and I have to say that in my experience that I have never met a psychiatrist who did not have delusions of godhood.
I have also had many clients/patients who came to the same conclusion.
Personally i do not think that doctors/psychiatrists are remotely interested in cultivating and empathic relationship with their patients or the staff below them.
Psychiatrists seem to regard their patients as being second class(or worse) I had one psychiatrist who said to me”Mr B……. you could never be my equal”
I have found this attitude prevalent throughout the NHS amongst doctors/psychiatrists.
So until there is a sea change of attitude and patients are given at least a modicum of respect the great divide between the deities and the lower species(everyone else) will remain.
I come from the generation that calls a spade a spade so I make no apologies for me somewhat sledgehammer comments.I am fully recovered now and have my own private practice. And sadly I have encountered the most appalling practices,abuses and attitudes towards the mentally one can imagine.
I just completed a webinar discussing this issue and cultural sensitivity toward African American Mothers. Glad to see people are talking about it………SMILES :) Love to connect with like minds.
Twitter: @jawspeaks