
The purpose of this rapid review was to scope through the current international guidelines on re-opening dental services to help policy and decision makers establish robust practical evidence-based guidelines.
Bottom Line
As the number of clinical guidelines and standard operating procedures increases, we are seeing a reduction in clear consensus regarding a clear way forward in patient management. If we are going to take an evidence-based approach in a land devoid of direct evidence the policy makers are going to have to defer to the clinical expertise and local knowledge of the profession in regards to the choice of PPE regarding Covid-19 negative patients requiring aerosol generating procedures.
Background
The recent ‘Cochrane Recommendations for the re-opening of dental services: a rapid review of international sources’ has been updated on the 16th May to include a further 5 international guidelines. The document now reviews 17 guidance documents from 16 countries (France, Spain, Portugal, Austria, Switzerland, Belgium, Netherlands, Norway, Denmark, Malta, America CDC, America ADA, Canada, Australia, New Zealand, India). The common themes and the relevant recommendations were divided into 5 domains:
- Practice preparation and patient considerations.
- Personal protective equipment (PPE) for dental practice personnel.
- Management of the clinical room.
- Dental procedures.
- Post-operative cleaning/disinfection/waste management.
Methods
The data was extracted in a similar way to the previous review. The five domains have mostly remained the same with little change in domains 1, 3, 4, and 5. The exception being domain 2 (PPE for dental practice personnel). The domain almost doubled in size to 29 subgroups from the original 15, but at the same time there was a reduction in the consensus with the mean dropping from 58% to 30% (See Figure 1.).
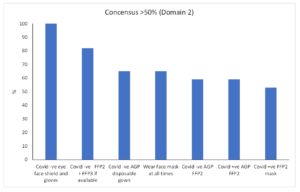
As with the previous review I selected the subgroups that achieved to filter out the large number of subgroups with a low degree of consensus. In the original paper there were 10 subgroups that scored ≥ 50%, in the update this reduced to 7 which constitutes a 42% reduction in agreement considering the expansion of the domain. (See Figure 2).
Figure 2. Subgroups with greater than 50% consensus.
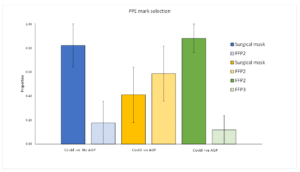
Looking at these subgroup headings there is a lot of duplication especially regarding the use of FFP2 and FFP3 masks and the infective status of the patient. To try and clarify this matter a subgroup analysis was undertaken (See Figure 3).
From this chart it was obvious that for Covid negative patients the consensus was for the use of surgical masks, and with Covid infective patients requiring an aerosol generating procedure (AGP) an FFP3 mask should be used. There was however a grey area around the use of a surgical mask combined with a face shield/visor, and an FFP2 mask for Covid negative patients requiring an AGP, the prevalence of asymptomatic patients being very low in the community (ONS, 2020). There was 41% (95% CI: 18% to 65%) agreement regarding the surgical masks, against 59% (95% CI: 35% to 82%) agreement for the use of an FFP2 mask, however as the sample size was small (n=17) the result was not statistically significant (p= 0.29).
Discussion
What can we conclude from the update? Due to the lack of hard evidence regarding the effectiveness of PPE in the real-world clinical environment the guidelines would appear to be based on opinion that ranges from the precautionary principle that all patients should be considered infective, to a more pragmatic approach based on the professions current cross infection strategies. In a perfect world we would like to see well design randomised controlled studies to answer these questions, but this does not address the here and now of real world dentistry. If we are going to follow the principles of evidence-based dentistry (Sackett et al., 1996) the clinicians are going have to make the decision of using surgical masks, or FFP2 masks for AGPs based on individual clinical expertise, best available evidence, and their patients values and preferences rather than rigid guidelines that can’t adapt to local circumstances.
References
Re-opening of dental services: A rapid review of international sources – update 16-05-2020
ONS. 2020. Coronavirus (COVID-19) Infection Survey pilot: England, 14 May 2020 [Online]. [Accessed 20-05-2020].
SACKETT, D. L., ROSENBERG, W. M., GRAY, J. M., HAYNES, R. B. & RICHARDSON, W. S. 1996. Evidence based medicine: what it is and what it isn’t. British Medical Journal Publishing Group.
Other references
Dental Elf 14th May 2020
Re-opening of dental services: A rapid review of international sources


Good info, I could be helpful to open my clinic