
The United Kingdom signed the United Nations Convention on the Rights of Persons with Disabilities (‘CRPD’) in 2009. The Convention is not yet part of English law in the sense that individuals can rely upon the rights that it contains before English courts. However, the UK has undertaken to bring English law into compliance with the CRPD. The UN body that has responsibility for monitoring the UNCRPD, the Committee on the Rights of Persons with Disabilities (‘Committee’) has made clear that it considers that, to do so, the UK must repeal legislation (i.e. the Mental Health Act 1983 and Mental Capacity Act 2005) that allow for involuntary treatment and detention of persons with disabilities on the basis of actual or perceived impairment.
In this debate piece, published yesterday in the British Journal of Psychiatry (Gosney and Bartlett, 2019), a psychiatrist, Dr Paul Gosney, argues that that the CRPD should either be amended to allow for the possibility of treating without consent those who lack capacity, or the UK should withdraw from the Convention. Professor Peter Bartlett, Nottinghamshire Healthcare NHS Trust Professor of Mental Health Law at the University of Nottingham, defends the Convention as a necessary challenge to the inequalities in the current system.
The debate piece takes the form of a structured initial challenge and response, followed by a further exchange.

The CRPD Committee has made it clear that if the UK wishes to bring English law into compliance with the CRPD, it must repeal existing mental health legislation.
Autonomy through compulsion and medication
Dr Gosney levels a number of charges against the CRPD (or, perhaps more accurately, the CRPD as interpreted by the Committee). He does so from the starting point that, whilst the CRPD does not mention mental illness, it is likely to fall within the definition of “psychosocial disability” used by the Convention, such that the implication is that no patient with schizophrenia can ever be admitted to hospital nor treated without consent, even in crisis situations. Dr Gosney identifies that attempts to retain the possibility of coercive treatment for those lacking decision-making capacity also fall foul of the Committee’s approach, the Committee considering that the assessment of mental capacity is flawed and represents another way of discriminating against those with disabilities.
Dr Gosney’s fundamental contention is that there is a subset of patients for whom the only way of maximising autonomy is through treatment with medication, even, in the last resort, under compulsion. Not allowing for this, he argues, places the CRPD in conflict with the positive duty on the State to protect life, highlighting the dilemma for a psychiatrist faced with a patient at risk of suicide.
Dr Gosney situates himself within his role as a psychiatrist, and acknowledges that he may be caught in an ideological view, but emphasises the dilemmas he faces when confronted with those who are unwell, present high risks to themselves, and are refusing help. Whilst he acknowledges the laudable aims of the CRPD, he believes that the parts of the Convention under consideration here risk damaging mental health patients by bringing back the pre-anti-psychotic era; if one of his tools is to be removed, he argues, there needs to be a corresponding commitment from society to do better by all its members. In the absence of such a change, he sees the choices as either amending the CRPD (or its interpretation) to allow for compulsory treatment, or withdrawing from the Convention.

Dr Gosney’s fundamental contention is that there is a subset of patients for whom the only way of maximising autonomy is through treatment with medication, even, in the last resort, under compulsion.
Human rights abuses and inequalities
Professor Bartlett acknowledges that the Committee’s approach is to put paid to mental health and mental capacity law as we know it. However, he seeks to place the Committee’s approach in terms of the CRPD as a whole, and why the Convention was thought necessary. He highlights a range of human rights abuses and inequalities faced by those with disabilities, emphasising that they are not just a foreign problem, but are issues that are very live in the United Kingdom. As he notes, the inequalities faced by those with disabilities have been with us so long that they feel natural, when they are not, instead representing policy choices taken in relation to a host of matters. He emphasises the extent to which they are choices, and based upon a characterisation of people with mental disabilities as appropriately the subject of control and social exclusion, leading to a world in which such people are second class citizens. In that context, the CRPD is an attempt to hit the reset button to enable people with disabilities to enjoy full and equal citizenship, and be placed in the same position as everyone else to make choices.
From that perspective, which Professor Bartlett suggests would be likely to receive broad support, he argues that the UK should not withdraw from the CRPD. He recognises the consequences for the law of its demands in relation to psychiatric treatment, but as he notes, it is a lot like how other medical services are provided. Further, if human rights are simply not getting through for people with disabilities, he suggests that the way forward cannot simply be a reaffirmation of what has gone before. Indeed, Professor Bartlett suggests that few psychiatrists and other mental health professionals would defend the status quo as a vision for the future.

Prof Bartlett highlights a range of human rights abuses and inequalities faced by those with disabilities, emphasising that they are not just a foreign problem, but are issues that are very live in the United Kingdom.
CRPD – a way for clinicians to deliver the services they want to deliver?
In their responses to each other, the two refine their positions, Dr Gosney ultimately restating his position that the ‘absolutist’ position of the Committee is impeding progress by requiring stakeholders to accept or reject the entirety of the Convention, and suggesting that the Committee respond in a more constructive way to the consensus that seems to be emerging around models based upon decision-making capacity.
Professor Bartlett identifies that the onus in terms of engagement lies not just with the Committee – the Royal College of Psychiatrists never having responded to any consultation preceding the issuing of a General Comment by the Committee; he further notes that the central requirement of the CRPD in this context is to start with the individual and what he or she wants (or would want), in fact, represents good clinical practice. He concludes that, perhaps, the CRPD represents a way for clinicians to deliver the services that they want to deliver.

The Royal College of Psychiatrists have never responded to any consultation preceding the issuing of a General Comment by the Committee.
What does the CRPD imply for the treatment of mental illness?
This debate summarises the core issues that are regularly seen as being at the heart of the question: what does the CRPD imply for the treatment of mental illness? Indeed, and – implicit in this debate, is there even such a concept as “mental illness”? Although neither of the participants in this debate address this, part of the challenge posed by the CRPD Committee is as to the very validity of the idea that mental distress can ever constitute an illness which either can or should be treated.
I say “CRPD Committee” here deliberately, because, as both participants allude to, there remains a live debate as to whether the Committee has derived obligations from the CRPD that are not, in fact, to be found in the Convention itself. It would perhaps have been helpful for the participants to have addressed this in a little more detail (see Martin et al, 2017). The easiest way of understanding it is perhaps to understand that, whilst the Committee (as the UN body established to oversee the Convention) is able to give the authoritative interpretation of its meaning, the Committee is not a court able to issue binding judgments. This has important consequences, because this means that the UN Committee is, in essence, a political body, which has to seek to persuade states that have signed the Convention, and courts examining the Convention in the courts of those states, of the correctness of its interpretation.

The CRPD Committee is not a court able to issue binding judgments.
Looked at through that light, the debate between Dr Gosney and Professor Bartlett shows that the Committee still has some considerable work to do to persuade those in positions of power, including clinical power. As Dr Gosney notes, the Committee did not persuade Sir Simon Wessely, the Chair of the Independent Review of the Mental Health Act 1983 which reported in December 2018, that the CRPD obliges the UK entirely to repeal the MHA 1983 or the Mental Capacity Act 2005 (Wessely, 2018). The Committee has also yet to persuade courts, including both domestic courts (i.e. the courts of individual member states) and the European Court of Human Rights that involuntary treatment or detention is incompatible with the Convention (AM-V v Finland, 2017; Roonan v Belgium, 2019).
However – and usefully drawn out by the iterative nature of the debate process recorded in the paper – there is perhaps more common ground between the ‘hard-line’ abolitionist view and the clinical view than might at first sight be apparent. Had there been a further iteration of the exchanges between Dr Gosney and Professor Bartlett, even more common ground might have emerged had the discussion engaged more of the positive duties upon states contained in the CRPD.

There is perhaps more common ground between the ‘hard-line’ abolitionist view and the clinical view than might at first sight be apparent.
The clue to this could be found in Dr Gosney’s observation that, if one of his (legal) tools as a psychiatrist is to be removed, there needs to be a corresponding commitment from society to do better by all its members. It is precisely this commitment that the CRPD demands through, for instance, the obligation it imposes upon states to secure the right to independent living for those with disabilities (Article 19) and the obligation that it imposes upon states to secure the right to health of those with disabilities (Article 25). If those obligations are carried through, and proper attention paid to the socio-economic factors underpinning mental ill-health, then it is not too much to suggest that the need for coercion will be dramatically reduced as the (perceived or actual) choice for clinicians such as Dr Gosney will not be between detention and watching a patient die.
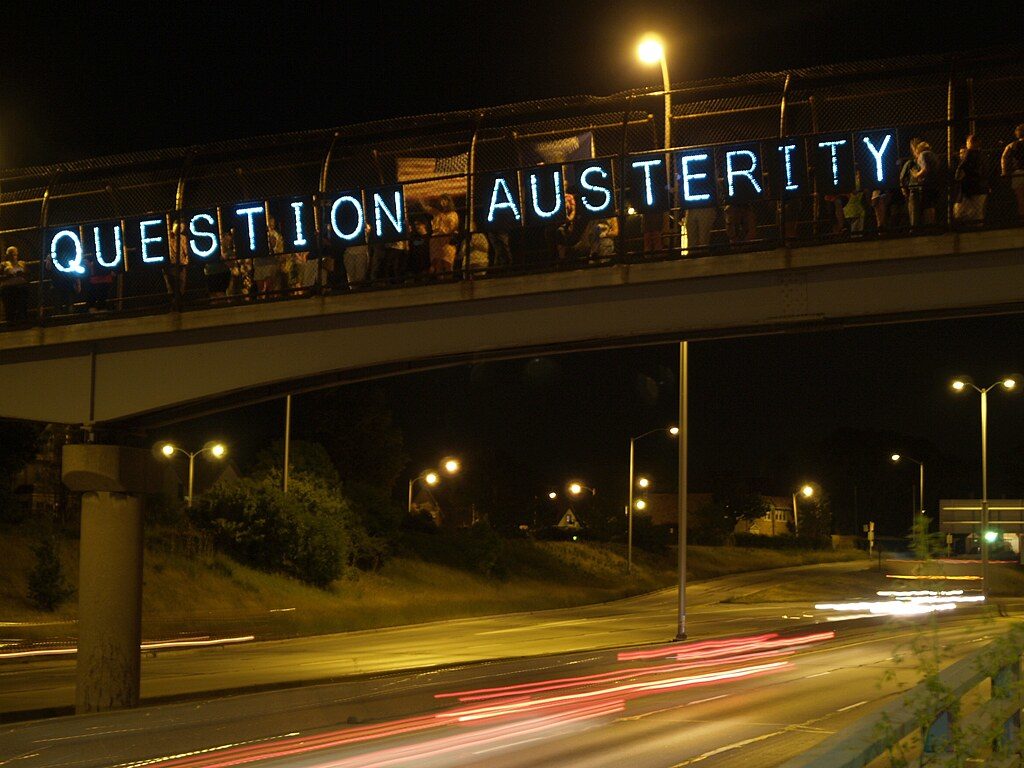
If proper attention is paid to the socio-economic factors underpinning mental ill-health, then it is not too much to suggest that the need for coercion will be dramatically reduced.
In this context, therefore, the debate can be seen as a useful summary of the first stage of the debates about the implications of the CRPD. The future direction of travel is hinted at as the two participants move towards each other in their responses. I would suggest it can then best be outlined in the report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health published on 24 June 2019 (Puras, 2019), and post-dating the writing of the article summarised here. The Rapporteur’s report, concentrating in particular on public health approaches and the socio-economic determinants of mental ill-health, sets out a route map towards the creation of non-coercive alternatives that respect the rights of persons with a lived experience of mental health conditions and mental health-care services (see also in this regard Gooding et al, 2018). The critical question, ultimately, will be whether it will be possible following this route map to entirely eliminate the need for a legal framework allowing for coercion as a last resort. If it is, then the arguments will fall away about whether the CRPD Committee is right to contend that the CRPD requires its elimination. If it is not, then those arguments will remain, but in relation to a very much smaller group of people and circumstances than at present.
Dainius Puras argues in his latest Special Rapporteur’s report that the promotion of mental health is a population-wide human right, not a luxury.
Conflicts of interest
Alex Ruck Keene was legal adviser to the Independent Review of the Mental Health Act 1983.
Links
Primary paper
Gosney, P., & Bartlett, P. (2019) The UK Government should withdraw from the Convention on the Rights of Persons with Disabilities. The British Journal of Psychiatry, 1-5. doi:10.1192/bjp.2019.182
Other references
Gooding et al (2018) Alternatives to Coercion in Mental Health Settings: A Literature Review. https://socialequity.unimelb.edu.au/news/latest/alternatives-to-coercion/
Martin et al (2017) Three Jurisdictions Report: Towards Compliance with CRPD Art. 12 in Capacity/Incapacity Legislation across the UK. Essex Autonomy Project: https://autonomy.essex.ac.uk/wp-content/uploads/2017/01/EAP-3J-Final-Report-2016.pdf
Puras, D (2019) Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health https://www.un.org/en/ga/search/view_doc.asp?symbol=A/HRC/41/34
European Court of Human Rights: AM-V v Finland [2017] ECHR 273 http://www.bailii.org/eu/cases/ECHR/2017/273.html
European Court of Human Rights: Roonan v Belgium [2019] ECHR 105 https://www.bailii.org/eu/cases/ECHR/2019/105.html
