
Commissioners and providers of health care will be interested in the learning shared in this new report, from Southwark and Lambeth Integrated Care (SLIC). SLIC is a programme and partnership created 4 years ago to develop integrated and proactive health care in response to increasing demand and a projected financial gap of £339 million.
All around the UK, decision makers are looking at ways to tackle similar problems. Health and care integration is widely seen as critical to person-centred care and the resilience of local communities. This report is an important addition to the evidence base, which is currently patchy. Much of the literature on integration is based on hypothesised benefits, so an evaluation which has tested some of those hypotheses is a significant contribution.
This learning report is based on an evaluation from Kings College London and offers actionable insights informed by a blend of empirical evidence and experiential learning. Anyone interested in integrated care will have seen umpteen case studies which can sometimes read more like policy spin than useable evidence.
Context
In 2012, SLIC was set up in response to growing fragmentation and a recognition that local systems were financially unsustainable. Supported by a charitable grant, which was key to enabling innovation and testing alongside a programme of quality improvement, SLIC set out to transform services to deliver more proactive care, centred around patients (rather than services) and which offered care in the most appropriate setting.

SLIC developed its own path to integration. Given the lack of evidence around at the time, they started their own programme.
Interventions
27 projects were developed by SLIC, focusing on aspects such as falls prevention, dementia and discharge planning. These were delivered alongside a number of projects developed by SLIC partners. Learning from mistakes early on in the transformation, SLIC emphasises the importance of co-design to ensure sustainability and to develop the relationships that underpin a well functioning health and care system. he programme team necessarily developed an adaptive and flexible approach, evolving the programme from an initial focus on the needs of over-65s to develop a resilience based approach.
Mechanisms
The SLIC team have helpfully condensed their learning into a Framework for Success:
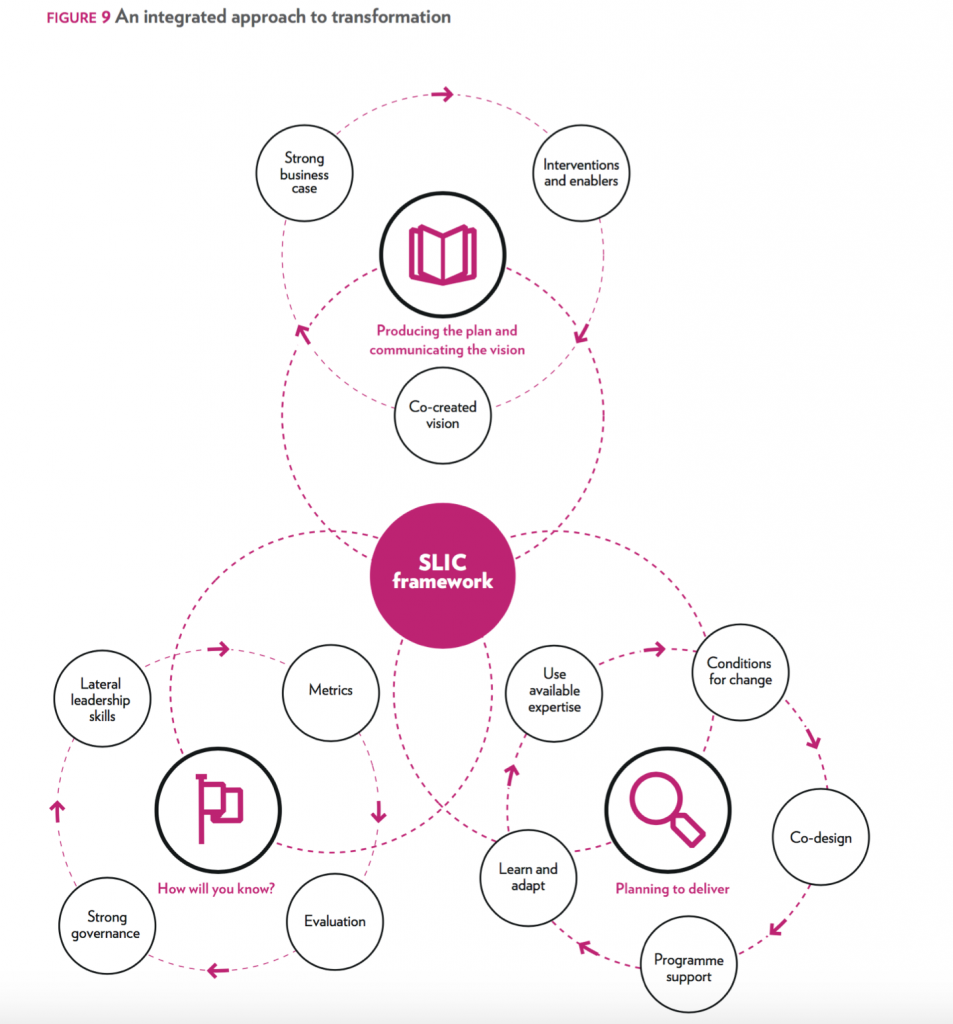
The SLIC framework comprising 12 key success factors. View bigger version of this diagram.
A key message throughout the report is that there are no short cuts or magic bullets; sustainable improvement is built on investment in people. Relationships, trust and leadership are emphasised as critical to releasing the expertise, enthusiasm and commitment (of staff, clinicians and citizens) which already exists within the local system. The team candidly admit that the programme only really gained traction when these were addressed.
Outcomes
Given the current climate, commissioners will undoubtedly be interested in the impact on unscheduled care and it would seem that SLIC has been able to stabilise emergency admissions and attendances in the last four years. The team suggest that whilst it has been relatively straightforward to demonstrate a positive impact on health outcomes and experience, it has been much more difficult to show savings.
And in fact, the programme team admit they had to revise original expectations and trajectories for savings, revising estimates from 14% to 5%. The evaluation does point to a shared view amongst stakeholders that the sustainability of the local health and care economy is much improved and there are examples of improvements such as the reduction of health needs assessments from 22 days to 6 days. Patient stories add a sense of real impact. There are a couple of areas which would be interesting to explore further; for example, the report talks about moving from a competitive provider culture to a collaborative culture.

The evaluation points to stakeholder views that the health system “is in a better place, taking together aspirations, relationships and service redesign”.
Reflections and implications for commissioners
The report makes interesting reading especially with its focus on how change was delivered rather than simply describing the interventions. There are some lessons here which are transferable to other contexts, notably:
- Working with stakeholders to develop the vision, case for change and to co-design interventions and outcome measures helped to turn around the top-down approach in the early days of the programme
- Stronger engagement can act as a reality check for expectations in terms of outcomes and timescales
- This can also help negate potential unintended consequences of moving from a medical to care model and the risk of clinical expertise being less integrated
- A more collaborative approach means system leaders need to provide stakeholders with the necessary time, space and resources
- Aligning with other initiatives is key as the programme can’t do everything. In this case, SLIC benefited greatly from the GP Emerging Leaders Programme which ran concurrently
- A structured approach to change led to a systematic approach to measurement and continuous evaluation and meant that interventions could only be taken forward if this was built in
- Stability of leadership is critical to relationships and building and maintaining credibility and momentum
- Consensus is rarely easy, but can be facilitated by a common direction of travel and a long term view.
Agreeing a sustainable strategy was not a linear path and consensus was at times been difficult to achieve.
Questions for leaders
The report raises 3 key questions which leaders will need to consider:
- What is the balance of the value proposition between cost saving, improving outcomes and improving patient and staff experience?
- What are the relative priorities between new models of care (such as falls prevention and care planning) and the enablers to support them, for example, information sharing and new forms of contracting?
- What are the timescales required for the delivery of benefits?
Links
Primary paper
Southwark and Lambeth Integrated Care (SLIC) (2016) Integrating Care in Southwark and Lambeth: What we did and how we did it.
Related documents
Wolfe C et al (2016) Southwark and Lambeth Integrated Care: Programme Evaluation. Report to SLIC Sponsor Board.
Photo credits
- Hywel Williams CC-BY-SA 2.0
- Prof Chen Hualin CC-BY-SA 4.0
- SLIC
- Campaign Bootcamp CC BY 2.0

Hi @charleswolfe16 We’ve blogged your SLIC Integrating Care report! Welcome any comments :-) https://t.co/U3EFoJ3vKd @ali_pals
Morning @slicareorg @MeravDover We’ve blogged your Integrating Care report! Welcome any comments :-) https://t.co/U3EFoJ3vKd @ali_pals
[…] Navigating the obstacles to health and care integration […]
Commissioners & providers of health care will be interested in the learning shared in this new @slicareorg report https://t.co/U3EFoJ3vKd
Important! @slicareorg say: no short cuts or magic bullets; sustainable improvement built on investment in people https://t.co/U3EFoJ3vKd
Actionable insights for health & care integration, informed by blend of empirical evidence & experiential learning https://t.co/U3EFoJ3vKd
Don’t miss: @ali_pals Navigating the obstacles to health and care integration https://t.co/U3EFoJ3vKd #EBP
Thanks, Alison. This is really useful. Especially as I’m just about to become the CEO of Age UK Lambeth!